Non Invasive Ventilation
Definitions:
CPAP: applies constant pressure throughout the breathing cycle to increase functional residual capacity (FRC) by recruiting alveoli, decreasing work of breathing, and improving oxygenation.
PEEP/EPAP: alveolar pressure before inspiratory flow begins. PEEP à decrease the amount of work required to initiate a breath and decrease atelectasis
Bi-level: Cycled ventilation between Inspiratory Positive Airway Pressure (IPAP) and Expiratory Positive Airway Pressure/PEEP. BiPAP supports ventilation and increases oxygenation.
Pressure Support: The difference between EPAP and IPAP is referred to as pressure support. Pressure support makes it easier to draw larger tidal volumes
BiPAP/ NIPPV/ Bi-level vs HFNC
· Oxygenation: Both devices can almost à 100% FiO2. HFNC à small PEEP ~5cm, max vs much higher PEEP on NPPV
· Work of Breathing: HFNC may wash out the anatomic deadspace à reduces the work of breathing. BiPAP can higher pressures and support majority of the work of breathing.
· Secretion clearance: Important in pneumonia to prevent mucus plugging improve clearance. BiPAP impairs secretion clearance, whereas HFNC does not seem to.
· Monitoring: Unable to communicate with patient effectively on BIPAP. BiPAP anxiety provoking and makes it difficult to differentiate between worsening clinical resp status vs anxiety. HFNC facilitates communication
NIPPV/Bi-level/ BiPAP
COPD
· Bi-level ventilation à decreases the risk of death (relative risk reduction 48%) and intubation rates (RRR 60%)
· Number Needed to Treat (NNT) for mortality benefit = 10
· NNT to prevent intubation = 4
· Furthermore, when comparing patients with moderate and severe acidosis, bi-level ventilation decreased mortality, rates of intubation, and lengths of stay.
· ** Ensure patient does not have a PTX that could tension once placed in PPV
Initial Settings:
- IPAP 8-20 cm H2O (up to 30 cm H20)
- EPAP 2-6 cm H2O to overcome intrinsic airway collapse
- Begin with either high IPAP and then titrate down, or low and titrate high.
SCAPE/ CHF exacerbation
· IPAP assists ventilation à decreases the WOB
· EPAP/PEEP increases the FRC by recruiting collapsed alveoli, improving oxygenation, and helping to force interstitial fluid back into the pulmonary vasculature
· Also, increases intrathoracic pressure à decreased left ventricular (LV) end diastolic volume à decreased afterload and increased LV ejection fraction/stroke volume.
· Common Initial Settings:
· IPAP: 10 to 20 cm H20
· EPAP: 5 to 10 cm H20
· I:E ratio of IT to ET and is usually set at 1:3 or 1:4 (Inspiratory to Expiratory ratio)
· Evidence for Bi-level ventilation in CHF exacerbations is unfortunately mostly supportive of CPAP with few trials comparing CPAP and BiPAP
· Cochrane review looking at NIPPV in CHF exacerbations à CPAP alone has been proven to decrease intubation rates and to decrease in-hospital mortality, without the same benefit seen using bi-level ventilation
· Lack of evidence does not mean lack of efficacy
How to assess your patients on NIV
· Oxygenation: good pulse oximetry waveform. ABG is rarely needed to measure oxygenation
· Work of breathing: The best metric is the respiratory rate. Worsening retractions, diaphoresis, tripoding, shallow breathing, and an abdominal paradoxical breathing pattern.
· Mentation: A patient who is easily arousible and mentating adequately doesn't have life-threatening hypercapnia
· BiPAP screen: Low tidal volumes and/or low minute ventilation àhypoventilation. But adequate tidal volumes and minute ventilation suggest a adequate response to NIV
· Treat the patient, not the ABG- Proven by Brochard 1995 (RCT) investigating the use of BiPAP in COPD: BiPAP improved mortality despite having no effect on ABG parameters after one hour à BiPAP can be successful without any immediate effect on the ABG.
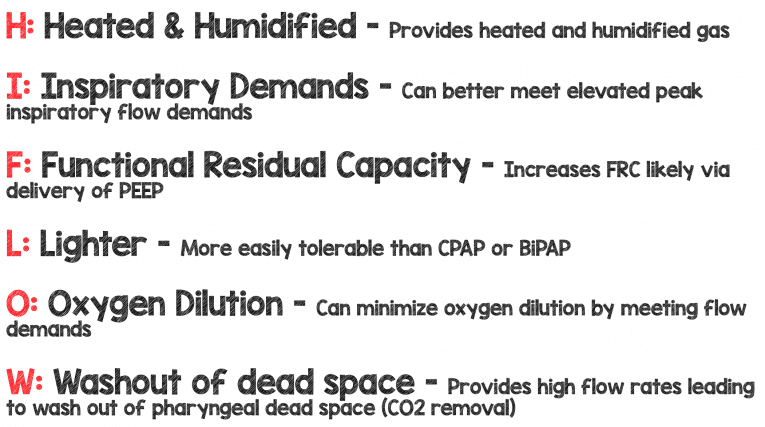
High Flow Nasal Cannula
· Low flow: NC ~ 1-5 L/min vs NRB ~15 L/min
· High Flow- 20-60 L/min
· Normal Resting breathing flow ~15-30 L/min
· Respiratory distress 60-180 L/min
Adult devices max out at 50-60 L/Min (max it out to start) and the dose for pediatric patient’s (based on trials) is 2L/Kg/Min
Maximize your devices flow rate initially then wean the fi02 to maintain your oxygen saturation goal
Adult Indications: Hypoxemic Respiratory failure (mostly Pneumonia) FLORALI Trial, DNR/DNI patients , Pre-oxygenation prior to Intubation
Pediatric Indications: Bronchiolitis, Asthma, Pneumonia, Croup
Take Home Points:
· Rule out pneumothorax (auscultation, US) prior to placing patients on NIPPV
· Do not base clinical management solely based off of an ABG esp if patient clinically improving
· Choose Bi-level vs HFNC based on patient’s diagnosis
· Best Metric to assess NIV success is respiratory rate
References:
Vital, F. M. R., Ladeira, M. T. & Atallah, A. N. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary oedema. Cochrane Database Syst. Rev. CD005351 (2013). doi:10.1002/14651858.CD005351.pub3
Frank Lodeserto MD, "High Flow Nasal Cannula (HFNC) – Part 1: How It Works", REBEL EM blog, August 20, 2018. Available at: https://rebelem.com/high-flow-nasal-cannula-hfnc-part-1-how-it-works/.
Frank Lodeserto MD, "High Flow Nasal Cannula (HFNC) – Part 2: Adult & Pediatric Indications", REBEL EM blog, August 23, 2018. Available at: https://rebelem.com/high-flow-nasal-cannula-hfnc-part-2-adult-pediatric-indications/.