If you remember one thing from this post remember this: up to 50% of dislocations spontaneously reduce before presentation to the the ER - these patients are STILL at high risk for neuromuscular injury. Take a good history about the mechanism of injury, get a good exam, and follow the instructions below, to make sure you dont miss a popliteal artery or peroneal nerve injury!
Diagnosis of Knee dislocation:
up to 50% of dislocations spontaneously reduce before presentation to the ER, but that doesn’t mean a neurovascular injury didn’t occur during the dislocation
consider the mechanism of injury: motor vehicle accidents, other high velocity mechanisms (falls, downhill skiing, football) make dislocation more likely
in rare cases, low velocity injuries in the obese, or sudden twisting motions in athletes can also result in dislocation
knee exam should focus on appearance, integrity/stability of joint, distal perfusion, and evaluating for peroneal nerve injury
peroneal nerve provides ankle dorsiflexion, toe extension, and sensation to first dorsal web space
usually 3 or more major knee ligaments must rupture for the knee to dislocation, so any knee exam w/multi-planar instability should be a suspected dislocation that spontaneously reduced
Anterior dislocation is most common (50-60%) named for the direction of translation of the proximal tibia
Posterior dislocation is even more commonly associated w/popliteal artery injury
Diagnosis of complications, especially in a spontaneously reduced knee:
most common injury is popliteal artery injury
presence of pulses does not exclude injury to the popliteal artery
if missed, can end up with AKA (delay of pop artery repair beyond 8 hrs invariably leads to limb amputation)
this is a highly litigated injury
ruling a popliteal injury via “hard signs” requires an immediate vascular surgery consult
hard signs include absence of pulse, pale or dusky leg, parasthesias and paralysis, rapidly expanding hematoma, pulsatile bleeding, bruit or thrill over the wound
There is no physical exam sensitive enough to rule out popliteal injury!!
quality of evidence behind ABI is poor as well
Wills et al prospective study suggests that normal ABI + period of observation w/no change in exam is 100% sensitive combination for ruling out vascular injury
Standard angiography is the standard of care
CT angio with runoff is next best test in the ER - ORDER THIS if concern for vascular injury
Management of a currently dislocated knee:
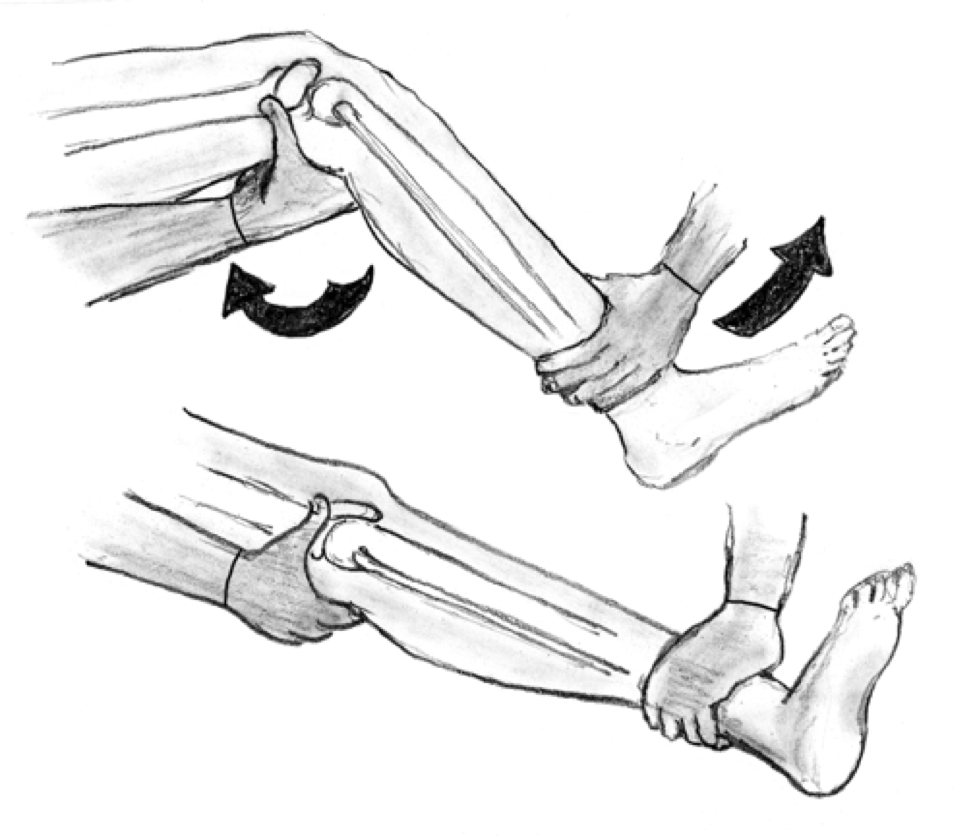
1. First and foremost the immediate reduction, and if neurovascular compromise exists – without radiographs.
a. Look for an anteriomedial skin furrow or “pucker sign” when the knee is extended – this signifies a posteriolateral dislocation, which are not reducible by closed reduction (require open reduction in OR).
a. Document neurovascular exam before and after reduction attempts
b. Initial approach should be application of longitudinal traction to lower leg (anterior dislocation may require additional lifting of distal femure, while posterior may require lifting the proximal tibia to complete reduction.
c. After reduction, the knee should be immobilized in a long leg posterior splint with the knee in 15-20 degrees of flexion
d. Again, these pts need either normal ABI with close monitoring and serial exams OR CTA to rule out vascular injury after initial reduction
References: