- Letter from the PD
- Program Overview
- Curriculum
- Resident Life
- Diversity & Inclusion
- Social EM
- Scholarly Tracks
- International
- Salary & Benefits
- Virtual Webinars
- How to Apply
- Interview Day
- Event Medicine Elective
Out of Hospital Care
Event Medicine Elective
Come join us in Brooklyn for the unique opportunity to provide medical care at various events around New York City!
Choose between a 2- or 4-week elective.
Offered from April through September.
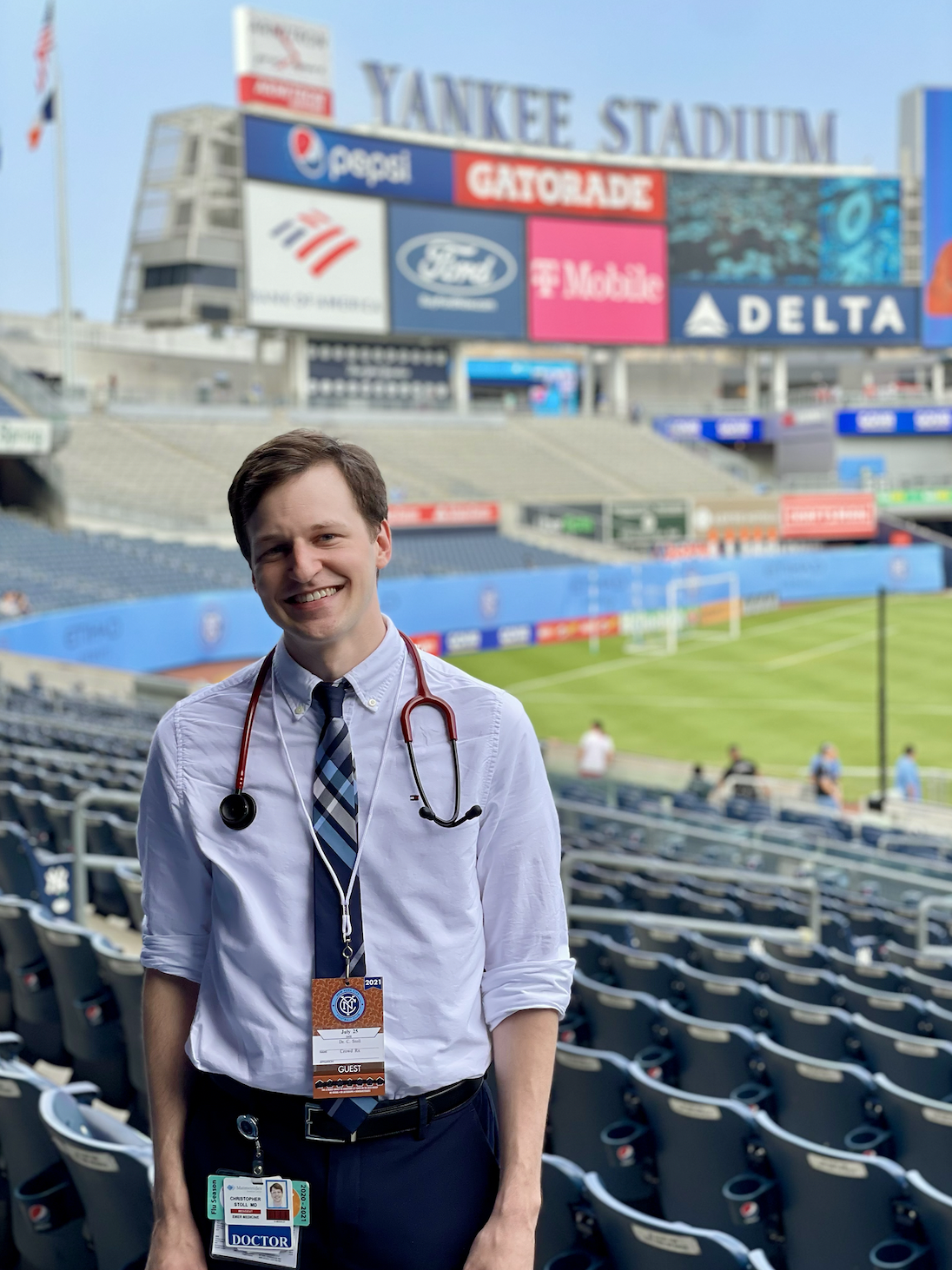
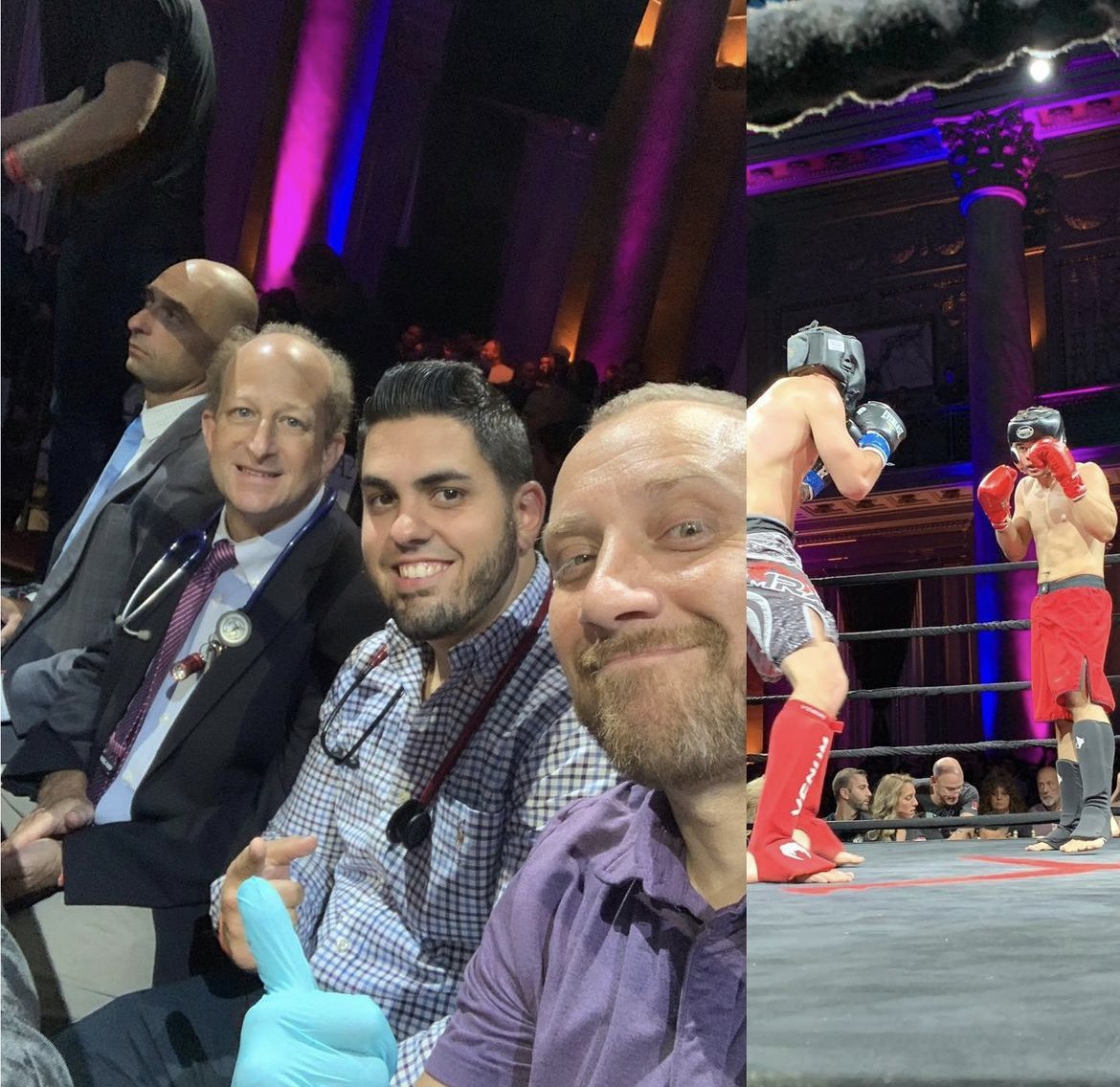
Be the lead physician on call at Yankee Stadium, Madison Square Garden, and other event spaces!
Practice resource utilization skills in the out-of-hospital setting.
For more information, please contact Dr. Matt Friedman (MattFriedman@maimo.org).
Goals and Objectives of the Elective
Mass gatherings generate a higher incidence of injury and illness than is expected from the general population despite typically being gatherings of healthy persons. The reasons for this are incompletely understood. While the majority of attendees who seek medical attention have minor injuries or illnesses and commonly remain at the event, deaths are not infrequently reported. At music festivals between 1999 and 2014, 722 deaths were reported. Thus, event medicine has become an integral component of mass gatherings, and provisions for onsite resuscitation are critical to improve patient outcomes. This elective will examine core principles of event medicine, analyze the variables that impact the Patient Presentation Rate (PPR) and Transport to Hospital Rate (TTHR) at mass gatherings, and offer interested emergency medicine senior residents hands on experience at daily mass gatherings in New York City.
Specific objectives include:
Understand the following concepts (MK, PC, P, C, SBP, PBL):
Legal and regulatory forces impacting EMS systems
The organization, administration and management of various EMS systems
Capabilities and differences between BLS and ALS providers
EMS protocol development and application
Integration of various EMS systems into the 911 system
Disaster preparedness and management
Triage and care of mass casualties
BLS, ACLS and PALS algorithms
Understand implications & legalities of “RMA” or refusal of transport. (C, P, SBP)
Be able to secure the airway and provide oxygenation and ventilation in the pre-hospital setting. (MK, PC, SBP)
Demonstrate understanding of the pathophisiology, diagnosis and management of overdose or toxicity from each of the following substances (MK): alcohols, cocaine, hallucinogens, mushrooms, opiates/opioids, sedatives/hypnotics, stimulants, and undifferentiated toxins
Understand the major toxidromes and be able to classify patients appropriately (MK, PC)
Display professional behavior: polite, respectful and mature behavior; enthusiastically pursue opportunities for patient care, arrive on time, honest, takes responsibility for errors, and assists other team members as needed.(P)
Assess, resuscitate, stabilize, treat and appropriately disposition any patient presenting for care in the pre-hospital setting as evidenced by demonstrating the ability to do each of the following physician tasks:
Rapidly conduct primary assessment and take appropriate steps to stabilize and treat patients. (PC, MK)
Communicate effectively to interpret and evaluate the patient’s symptoms and history; identify pertinent risk factors in the patient’s history; provide a focused evaluation; interpret the patient’s appearance, vital signs and condition; recognize pertinent physical findings, perform techniques required for conducting the exam. (PC, MK, C)
Recognize age, gender, ethnicity, barriers to communication, socioeconomic status, underlying disease, and other factors that may affect patient management (MK, SBP)
Demonstrate principles of professionalism: polite, respectful and mature behavior; enthusiastically pursue opportunities for patient care, arrives on time, honest, takes responsibility for errors, and assists other team members as needed. (P)
Demonstrate understanding of ethical and legal concepts pertinent to patient management. (P)
Develop a differential diagnosis and establish the most likely diagnosis in light of the history, physical, interventions and test results.(MK)
Select, obtain informed consent when necessary, and perform all procedures and non-pharmacologic therapies (PC, MK)
Select appropriate pharmacotherapy, recognize pharmacokinetic properties, and anticipate drug interactions and adverse effects. (MK)
Evaluate and reevaluate the effectiveness of a patient’s treatment or therapy, including addressing complications and potential errors.
Collaborate with physicians and other professionals to evaluate and treat patients, arrange appropriate placement and transfer if necessary and communicate effectively with patients, family and involved health care members. (C, P, SBP).
Schedule
During this two- or four-week rotation, residents will participate in the following activities:
Orientation and introduction to principles of mass gathering event medicine by Dr. Friedman
Twice-weekly formal didactics delivered by EMS fellows and board-certified EMS faculty members on prehospital care, trauma, and toxicology as relevant to the practice of event medicine.
Attendance at weekly Emergency Medicine residency core conference, either at Maimonides or at home residency program.
Experience in medical coverage at approximately four events per week averaged over the duration of the rotation. Events may take place at Madison Square Garden, Yankee Stadium, or other venues in the New York City area. Events outside of the New York City area may be available for medical coverage, depending on the time of year of the rotation.
Application Process and Requirements
This elective is only offered from April to September.
Must be a current Emergency Medicine resident in the final year of training at an ACGME-accredited program by the time of the rotation start date.
A completed application and letter of good standing written by the Program Director must be submitted no later than THREE MONTHS prior to the anticipated start date of the rotation. Applications and letters should be emailed to Susan Caliendo (SCaliendo@maimo.org) and Matt Friedman (MattFriedman@maimo.org).
All applications will be reviewed on a rolling, first-come, first-served basis.
If accepted for the rotation, applicants must be able to complete all required credentialing information in a timely fashion in order to start. Participating institutions will be required to complete a Program Letter of Agreement with Maimonides Medical Center.