One of my favorite topics that is as nerdy (if not more so) than toxicology is a subspecialty of cardiology called electrophysiology. While I am not an expert at any field at this point, I certainly enjoyed learning from our prestigious faculty in the CICU. This is the first of a 2 part pearl of the day. The next pearl of the day, we will get into the various modes of pacemaking and what they mean.
So let us review: pacemakers, AICD’s, the different varieties, why people have them, and what we as ED providers need to know.
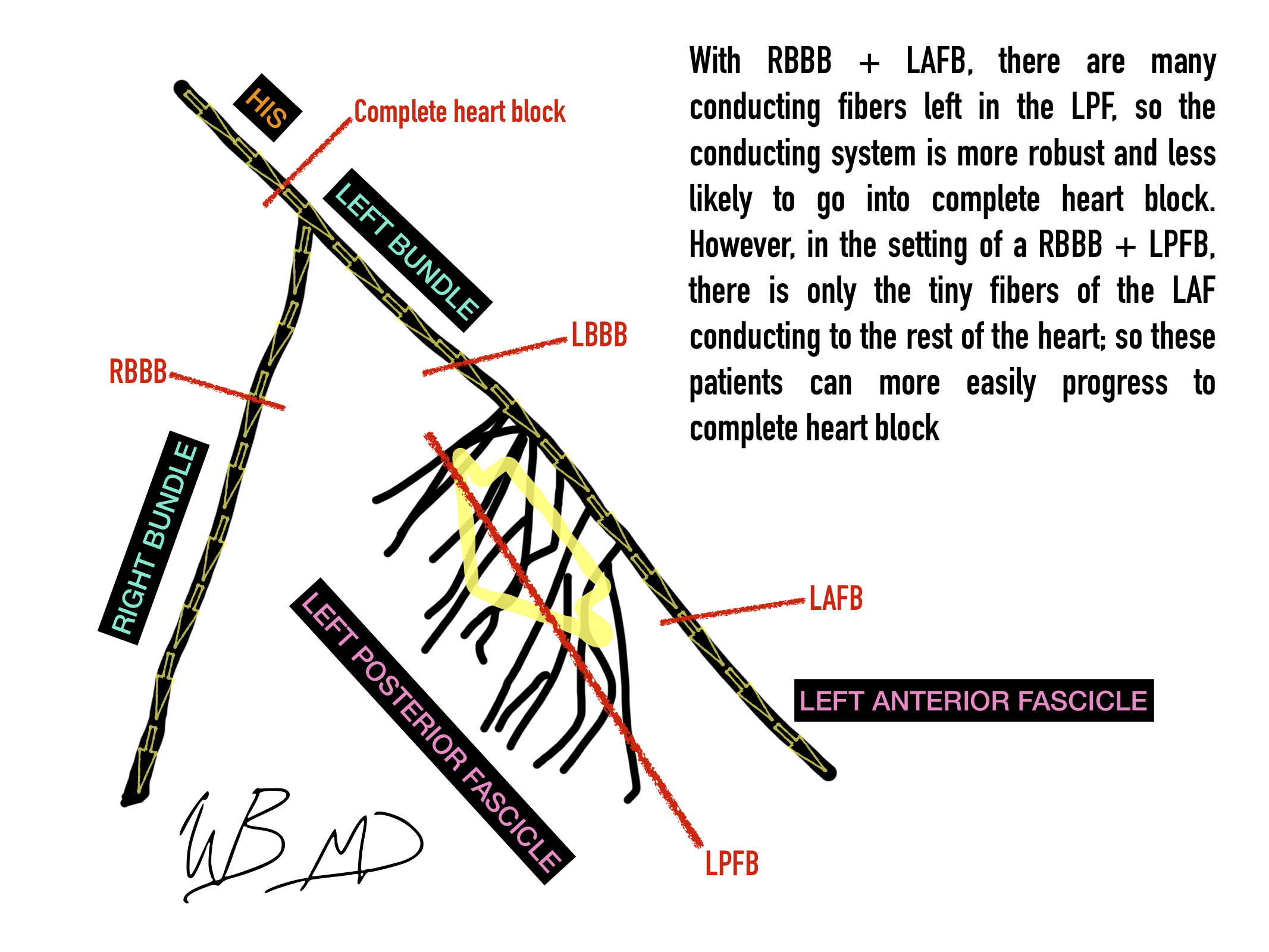
Electrical Conduction system of the heart
I have attached an infographic showing the various points of heart block. Notice how the left posterior fascicle has many conducting fibers. This important, because in the setting of RBBB + LAFB, there are many conducting fibers left so the conducting system is more robust and unlikely to go into complete heartblock. However, in the setting of a RBBB + LPFB, there is only the tiny fibers of the LAF conducting to the rest of the heart; so these patients need a pacemaker.
Pacemakers
Complete heartblock or ecg findings that they will likely soon develop complete heart block (eg mobitz type 2 and combined RBBB with left posterior fascicular block) are indications for pacemaker placement. If they are unstable on presentation, they need an emergently placed transvenous pacer.
A single lead pacemaker tunnels through the venous system and delivers electrical impulses to the right ventricle. The wave of depolarization starts in the right ventricle; thus, the ECG finding of a paced rhythm is of a widened QRS seen in a LBBB.
For patients with reduced EF’s who need pacing, there is a current trend to place biventricular pacemakers. With these devices, a lead is placed into both the right and left chamber of the heart. This is termed cardiac resynchronization therapy (CRT). Because both the chambers of the heart are paced simultaneously, the QRS narrows and it is thought this improves EF.
Automatic implantable Cardiac Defibrillators (AICD’s)
There are various models of AICD’s and are capable of providing single chamber pacing and CRT in all of the various modes depending on model. There main function is to monitor the heart for dangerous arrhythmia and deliver electrify to abort the dangerous rhythm (usually tach or vfib).
Aside from there pacemaking and/or automatic defibrillator function, all of these devices are essentially continuous cardiac monitors. As such, any patient who has one of these devices who presents to our ED can have there device interrogated.
Mostly for the interns: any syncope, report of AICD discharge, palpitations, etc with an implantable device should have there device interrogated.
Special note: placing a magnet on an AICD will turn off the defibrillator mode. This should be performed after a failed resuscitation or in a DNR/DNI patient at the point of death.