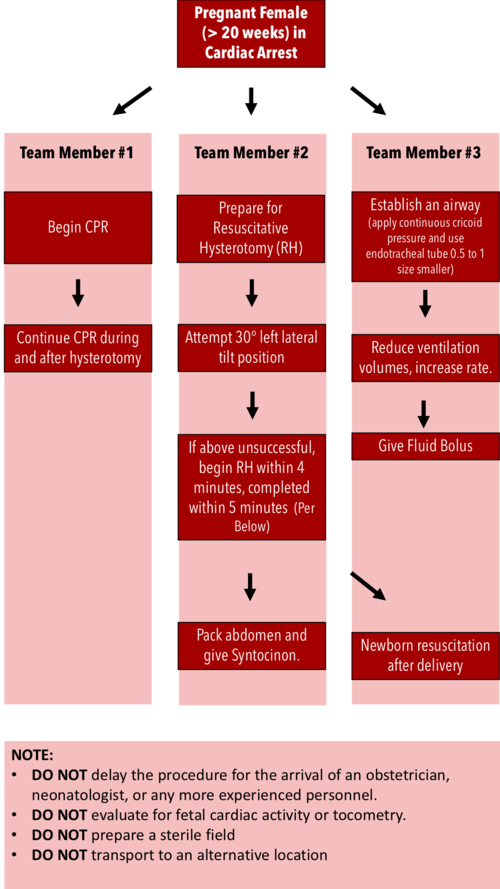
Formerly known as the perimortem cesarean section, the resuscitative hysterotomy is performed in a pregnant patient of > 20 weeks gestation in cardiac arrest to improve the chances of ROSC.
Forget about the 4-Minute and 5-Minute rule!
Even in controlled simulations with obstetric teams, timing has been problematic.
While the procedure should be performed as quickly as possible to improve outcomes, there is generally no contraindication to performing the procedure beyond the 5 minute mark.
The procedure has benefited pregnant patients up to 15 minutes and fetuses up to 30 minutes after maternal cardiac arrest.
DO’s and DONT’s
DO assign team roles and prepare all equipment prior to patient arrival
DO start chest compressions immediately, establish an airway, and get IV access
DO give fluids
DO give blood in the setting of trauma
DO NOT stop to evaluate for fetal cardiac activity or tocometry
DO NOT prepare a sterile field (but be as clean as possible)
DO NOT wait for OB/GYN to arrive before starting the procedure
DO NOT transport the patient to another location
THE PROCEDURE
Drench the abdomen in betadine and get ready to cut
With a scalpel, make a vertical incision from the xiphoid process down to the pubic symphysis, cutting through the skin, fat, fascia, and peritoneum
Avoid cutting the bladder — find it, and retract it
Blunt dissect down to the uterus
Make a vertical incision in the uterus large enough to fit 2 fingers in
Once inside, lift the uterine wall with your fingers
Use blunt scissors to divide the uterus between your fingers and extend the incision
Deliver the fetus
Double clamp the umbilical cord and cut BETWEEN the clamps
Deliver the placenta
Wipe the endometrial cavity clean with a clean, moist lap pad
Pack the uterine cavity with sterile towels
Continue resuscitation
WATCH EMCrit VIDEO of a LIVE SIMULATED RESUSCITATIVE HYSTEROTOMY
https://www.youtube.com/watch?v=IwDWv2iyAos
SOURCES
Tintinalli’s Emergency Medicine, 9th Edition pp 646-647
Rose, C.H. et al, Challenging the 4- to 5-minute Rule: From Perimortem Cesarean to Resuscitative Hysterotomy Obstetric Anesthesia Digest December 2016 - Volume 36 - Issue 4 - p 171
WikiEM: Resuscitative Hysterotomy