Unstable Bradycardia
Background
· HR less than 60 BPM
· Not all bradycardia is bad and scary, some presentations are benign and asymptomatic
· Broad differential, some examples include:
Cardiac (structural/EP): AV block, STEMI, CHD, CM, Aortic dissection, etc.
Respiratory: Hypoxia, resp failure
Infectious: Myocarditis (viral), Lymes dx, etc.
Metabolic/Endocrine: electrolytes, hypothyroidism/myxedema coma, hypoglycemia, hypothermia, heat exhaustion/stroke
Tox/iatrogenic: BB, CCB, Dig, Clonidine, Opioids, TCAs, Keppra, Amio, etc.
Trauma: increased ICP, spinal injury
· Place pacer/Zoll pads on patient
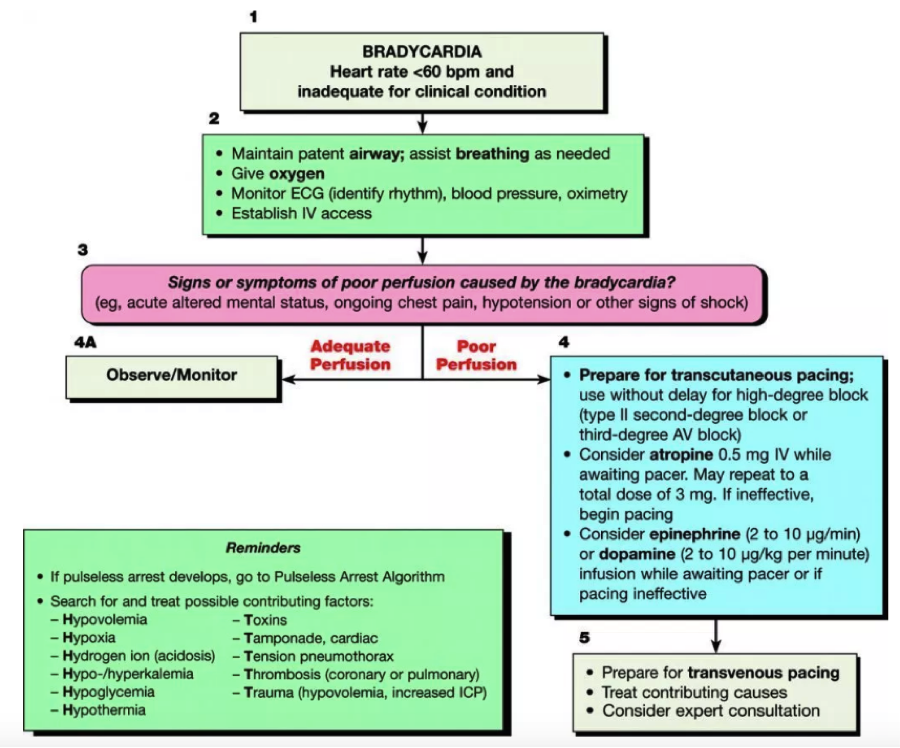
· ACLS guidelines for bradycardia exist
Unstable patient
· ABCs
· Don’t let the patient D.I.E
Think drugs, ischemia, electrolytes
· Place on monitor and obtain access
If cant get an pIV, then try IO or central line
*send for labs, VBG/BMP asap. Looking for electrolyte derangements (hyperK) that can change management
· Place transcutaneous pacer pads so you’re ready to pace at any moment
Anterior/posterior position best
· Try atropine
Doesn’t hurt to try, may work
.5mg IV, can be repeated q3min to a max dose of 3mg
· If atropine is not working, high probability it wont, then start transcutaneous pacing while getting chronotropic medication (pressors) ready and then titrating to desired effect
Place dial on pacer mode
Set pacer rate >30BPM above pts intrisic rhythm (usually 60-80 BPM)
Set mAmp on 40, increase by 5mAmp as needed
Monitor for capture
Electric capture: downward pacer spike followed by wide QRS
Mechanical capture: palpate pulse and correlate with monitor/pulse ox
Try to give pt something for pain
Get ready to place a TVP
· Pressors
“For symptomatic bradycardia or unstable bradycardia IV infusion a chronotropic agent (dopamine & epinephrine) is now recommended as an equally effective alternative to external pacing when atropine is ineffective.”
Thought: takes time to draw up meds/titrate. start external pacing. Get meds ready and administer, especially if hypotensive.
Can start either Epinephrine 2-20 micrograms/min or Dopamine 2-20 micrograms/kg/min, titrate accordingly
If epi/dopamine don’t work separately, then try them together
If bradycardia still not improving, then try isoproterenol 2-10mcg/min
Isoproterenol is an analog of epinephrine
· Additional medications to consider
Digoxin
Send dig level
Consider digibind
CCB
Calcium gluconate, high dose insulin
BB
Glucagon, high dose insuli
Organophosphates
Atropine, pralidxime
· STEMI?
Usually inferior wall MI
Advocate for pt to go to cath lab