Developing para/quadriplegia as a result of a spine injury is a devastating event. Such injuries place an enormous emotional, social, and financial burden on the individual and society. Remember there is only meager evidence that steroids improve acute spinal cord injury (ASCI) outcomes in any meaningful way (see NASCIS trials). Until better therapies are developed (perhaps through stem cell research), there is currently no ideal treatment for ASCIs. Until future therapies are developed, the best approach is to prevent, identify, and repair existing spine fractures before injury to the spinal cord occurs. Through the use of judicious immobilization, clinical judgment aided by clinical decision instruments and the use of radiography, the astute emergency physician will identify these spine fractures. This will prevent secondary cord injury, allowing early surgical repair. Source: Ebmedicine.net
Spinal cord syndromes are usually the result of conditions extrinsic to the spinal cord, such as: compression due to spinal stenosis, herniated disc, tumor, abscess, and trauma (i.e. hematoma, retropulsion of bony fragments, bullet/knife injury).
Less commonly, disorders intrinsic to the cord, such spinal cord infarction or hemorrhage, transverse myelitis, viral infection (HIV, polio, West Nile), syphilis, vitamin/mineral deficiency (B12, copper), decompression sickness, lightning injury, radiation therapy, syrinx, and neoplasms can also lead to the characteristic syndromes highlighted below.
Lastly, we must not forget about the commonly tested synaptic diseases that may present with a variable degree of weakness and/or sensory findings. Consider these zebras in your differential: tick bite paralysis, MG, Lambert Eaton Syndrome, Guillan-Barre, and Botulism.
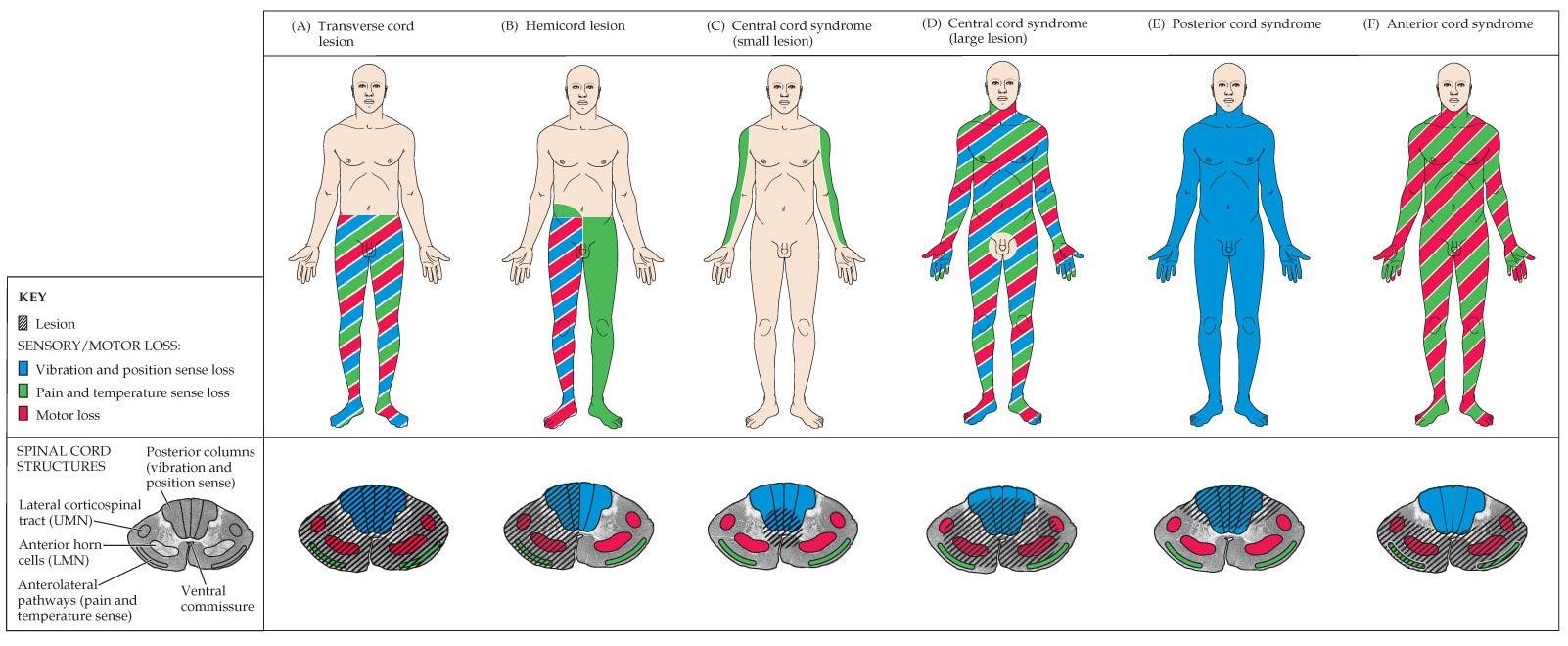
- Transverse cord lesion – Can be caused by hemisection of the cord usually in the setting of penetrating trauma. Results in loss of all function (vibration/proprioception, pain/temperature) below the level of the injury.
- Hemicord lesion a.k.a. Brown-Sequard’s paralysis - resulting in loss of motor and proprioception below the ipsilateral side as the injury or lesion, and loss of pain and temperature sensation below the contralateral side as the lesion. Note patients will have loss of pain and temperature sensation on the ipsilateral side at the level of the lesion as well given the crossing of the fibers in the cord.
- Central cord lesion (most common) – typically from a hyperextension injury. Results in upper extremity motor and sensory loss in a cape-like distribution. Syringomyelia can also cause this but classically presents as loss of pain/temperature sensation in a cape-like distribution only.
- Central cord syndrome – Same as above but larger. Devastating injury, complete paralysis. Sacral sparing may occur.
- Posterior cord syndrome – A common result of a hyperextension injury. Also, classically “Tabes Dorsalis” from syphilis and “Subacute Combined Degeneration” from B12 Causes loss of vibration and position loss below the level of the lesion, and affects the lateral cords in B12 deficiency leading to further sensory loss. Don’t forget to do a Romberg test!
- Anterior cord syndrome – Usually caused by ischemia to the anterior spinal artery (ASA) or post AAA repair, or flexion injury such as diving injury at C5-C7. Results in motor function and pain/temperature loss below the level of the lesion. Worst prognosis.
