We’re going to go though this POD as a case rather than me yelling facts at you. READ ON!
Red phone rings. “We’re bringing in a STEMI. Vitals are HR 155, BP 75/55, RR 35, 90% on NRB. Our prehospital EKG should be in the email system already.” Cath lab fellow is notified.
The patient is brought into resus. Middle aged man, diaphoretic, holding his chest, tachypneic but no accessory muscle use. “Help me doc. I think I’m dying. My chest hurts so bad and I can’t breathe… What’s that? No I don’t take meds or have medical problems but I don’t really see doctors either.”
You listen to his lungs: crackles b/l; ultrasound his lungs: B-lines b/l… seems like acute pulmonary edema but he’s hypotensive so nitro’s out of the question. Furthermore, looks like it could be RV MI. You call for BiPAP (cautiously because that could make him more hypotensive too), which he tolerates and he feels better. A small dose of fentanyl helps with his pain as well.
Meanwhile, cardiology is busy consenting him for cath lab, you put in orders, and labs are being drawn. Another EKG and set of vitals are repeated, essentially the same as prehospital.
Chest X-ray shows up and shoots an image.
Oh damn, this guy really does have pulmonary edema. Why does this guy have acute pulmonary edema? You astutely go back and put the probe on his chest again to look at the heart.
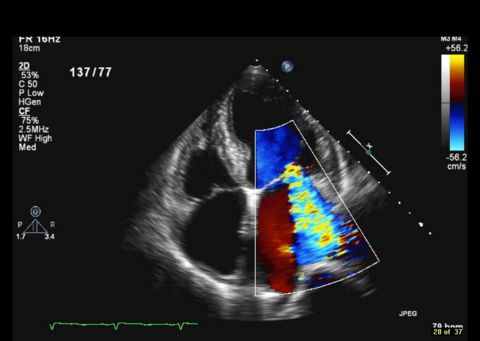
His parasternal window is garbage but his apical window is decent. Below is your apical long (same probe orientation as parasternal long but in the apical position).
...there’s something flapping around on his mitral valve… it’s his papillary muscle! This guy ruptured his papillary muscle!
Papillary muscle rupture
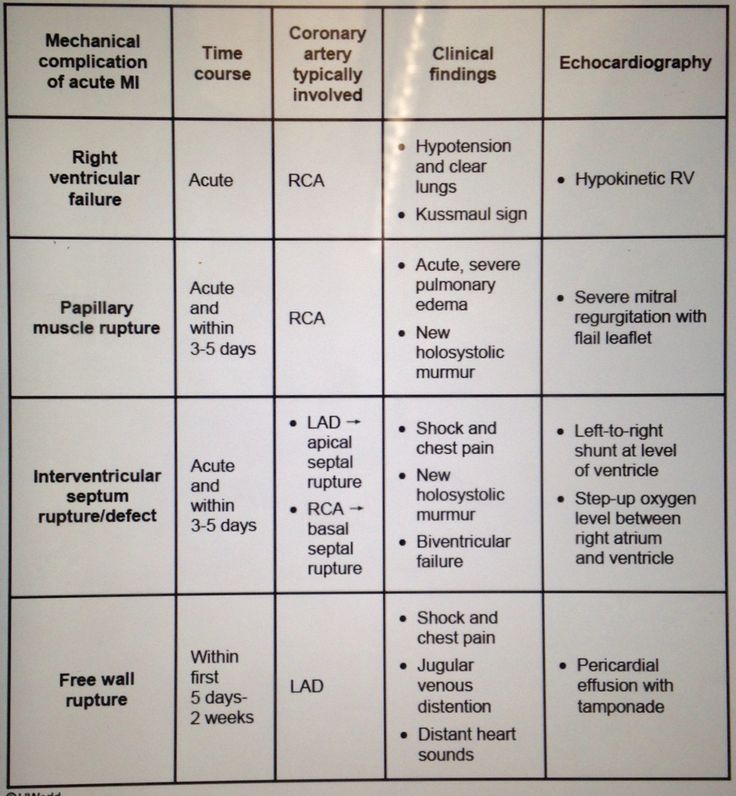
… you have a sudden flashback to studying for USMLE Step 1. A table that you once studied comes to your mind…
Right! It’s one of the
mechanical complications of acute MI
… happens with
RCA infarcts
, can happen
acutely and within 3-5 days
…
acute severe pulmonary edema with flail leaflet on the echo
... bad news…
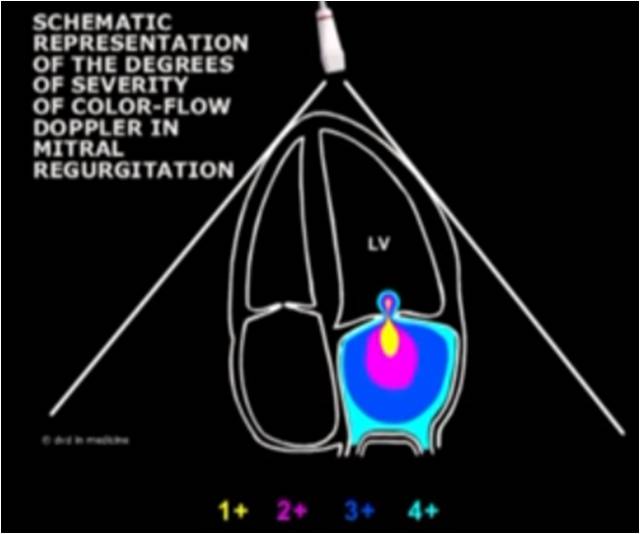
Your flashback ends and you’re back in the ED ultrasounding this guy. His mitral regurgitation is pretty insane when you put some color on it.
Probably 4+
Suffice it to say, cardiology doesn’t want to take him to the cath lab any more, but at least the fellow documents an official echo to back you up. You change your underwear and
call cardiothoracic surgery
. They’re booking him for the OR immediately to repair his valve.
As an academic exercise, you and the cardiology fellow take a second to listen to his murmur. God forbid you had to diagnose this without ultrasound.
There it is,
holosystolic at the apex
.
He’s still hypotensive though and now he’s getting a little altered. The OR isn’t ready yet.
If he wasn’t hypotensive you could use nitroprusside to reduce his afterload
and improve his forward cardiac output… but since he’s hypotensive, cardiology helps you set up the only
other option: an intra-aortic balloon pump
to support perfusion to his heart and brain until surgery.
Off to the OR he goes. His operative mortality is 50% but it’s his best shot. With medical therapy alone, his mortality would be 75% at 24 hours and 95% at 2 weeks.
Well done, doc. He has a fighting chance now.