Where to start?
First, figure out is it monocular or binocular diplopia?
Monocular: diplopia persists with one eye closed
Almost exclusively an eye problem. It is almost always benign and most often due to refractive error. Give ophthalmology referral and no further imaging is indicated unless warranted by other signs or symptoms.
Binocular: diplopia resolves with one eye closed
Often due to neuromuscular dysfunction causing misalignment of gaze.
This requires further evaluation in the ED to rule out acute neurological injury.
Next, is the diplopia isolated or associated with other neurologic signs or symptoms?
Do a thorough neurological exam.
If you find any other neurological symptoms or signs, consider a stroke code/consult and get CT/MRI.
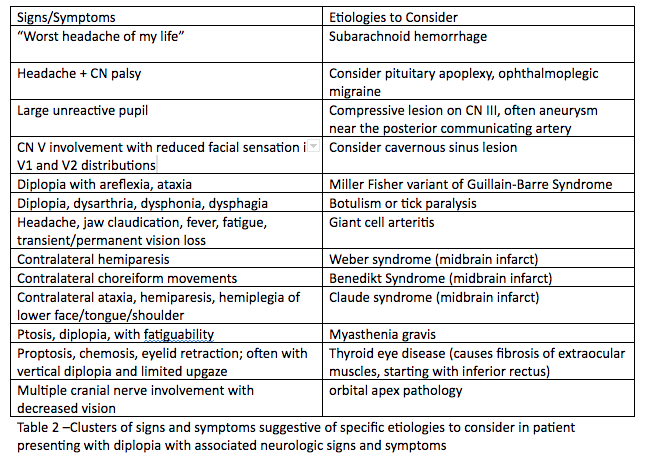
Think of the following table of diagnoses for patients presenting with diplopia and focal neurological deficits, and order the appropriate tests and imaging needed:
If there is an isolated palsy, try to localize the lesion.
Isolated 3rd nerve palsy: may be due to a cerebral aneurysm, especially if affecting the pupil, and must be emergently evaluated with noncontrast head CT and CTA.
Isolated 4th nerve palsy: usually present with vertical or diagonal diplopia, usually due to trauma or idiopathic; be sure to check for cerebellar signs because the 4th nerve exits on the dorsum of the brainstem and can be compressed by a posterior fossa tumor. If no cerebellar signs or trauma, can be discharged with an ophthalmology referral.
Isolated 6th nerve palsy: present with horizontal diplopia, usually idiopathic, check for bilateral 6th nerve palsies as this can be a sign of a tumor (some sources state an isolated 6th nerve palsy should also be evaluated with head imaging prior to dispo).
For horizontal diplopia, evaluate for internuclear ophthalmoplegia, and if present, get an MRI. Various causes, including multiple sclerosis.
In children, there is a higher prevalence of malignancy (vs microvascular insult) so they always require head imaging.
Now what?
The need for neuroimaging in diplopia will depend on the palsy the patient has as well as the presence of other abnormalities in the history or physical exam.
Isolated 4th nerve palsies and 6th nerve palsies can be referred to a specialist for evaluation and do not require imaging in the ED (except as outlined above).
The presence of a 3rd nerve palsy, multiple concomitant palsies, evidence of papilledema, infection, trauma, or cavernous sinus thrombosis require urgent imaging in the ED.
3rd cranial nerve involvement: CTA
Increased ICP: CT head
Associated neuro deficits/complex motility disorders: CT head, preferably MRI
Suspected infection: CT head/orbits with contrast
Suspected Cavernous Sinus Thrombosis: CTV, followed by MRV if CTV negative
Patients over age 50 with diplopia should have inflammatory markers ordered.
Diplopia merits urgent referral to an ophthalmologist or neurologist once immediate, intervenable causes have been ruled out.
Sources
http://www.emdocs.net/diplopia-evaluation-and-management/
https://www.nuemblog.com/blog/double-vision
https://crashingpatient.com/wp-content/uploads/2018/06/diplopia.pdf