Monday marks the start of a new week, and I thought I'd start us off with a more cheery and uplifting topic.
Death!
Technically contains spoilers, but well-foreshadowed (obvious) ones.
Episode 4 concludes the story of nursing home resident Mr. Spencer, whose wishes against intubation had been ignored until now; and also trundles towards the inevitable end for Nick Bradley, whose heart is pumping but has shown no other signs of life, and is undergoing repeated rounds of brain death testing in the ED.
In an act of (delayed) mercy, Mr. Spencer is extubated in line with his original advanced directives and allowed to progress to circulatory death. This form of death is the oldest and most "obvious" type, with it fundamentally boiling down to "the heart stopped" (and in today's high-tech world, we can add verbiage like "cardiac standstill or no organized cardiac activity on echo"). For the purposes of medical documentation, there must be another cause of death listed — saying a patient died of "cardiopulmonary arrest" is akin to saying "they died because they died". In Mr. Spencer's case, we could perhaps list "septic shock", "acute hypoxic respiratory failure", "pneumonia", and "advanced age" as his causes of death. Circulatory death is sometimes reversible with cardiopulmonary resuscitation, which creates an interesting ethical conflict with regard to the "Dead Donor Rule" in organ donation. The 1981 Uniform Determination of Death Act, which has been adopted by most states in the USA, requires "irreversible cessation of circulatory and respiratory functions" in order to declare death; meanwhile, the ethical norm of the DDR requires all donors be dead — so is your potential donor really dead if CPR has a chance of resurrecting them? The current widespread practice is to respect the pillar of autonomy, i.e. if ceasing or withdrawing care according to the wishes of the patient or decision-maker would lead to death, then that would be functionally "irreversible". (I also invite everyone with more of an interest in ethical debates to consider the classical Trolley Problem)
On the other side, the brain death testing for Nick Bradley continues. He's a young man who suffered anoxic brain injury after an unintentional opioid overdose (from contaminated alprazolam). His neurological exam was dire, with dilated and fixed pupils, no corneal reflex, no gag reflex, no oculocephalic reflex (eye movements with head turning) or oculovestibular reflex (eye movements with ice water in ear). The UDDA also creates the standard that the entire brain (including the brain stem) must lose function in order to declare brain death. There is no unifying federal guideline for how testing for brain death can be done. Protocols are based on state regulations and institutional policies, and two states (NJ and NY, as I'm sure many of you have seen) have provisions for the restriction of brain death testing. In Nick's case, as the brain stem controls respirations, an apnea test was performed in a prior episode to evaluate his respiratory drive. He is part of the population that the test is valid for: otherwise without prior respiratory disease, and with no hypoxemia, acidosis, hypotension, or hypothermia. An ABG is obtained first to check baseline PaCO2, then the vent is adjusted to provide oxygen without ventilation (e.g. CPAP mode with no backup rate). This state should be continued for 10 minutes, and aborted if the patient shows any signs of spontaneous breathing or decompensation; at which point another ABG should be taken. If the pH < 7.30 and PaCO2 > 60 (or >20 above patient's prior baseline, if abnormal), there is no respiratory drive.
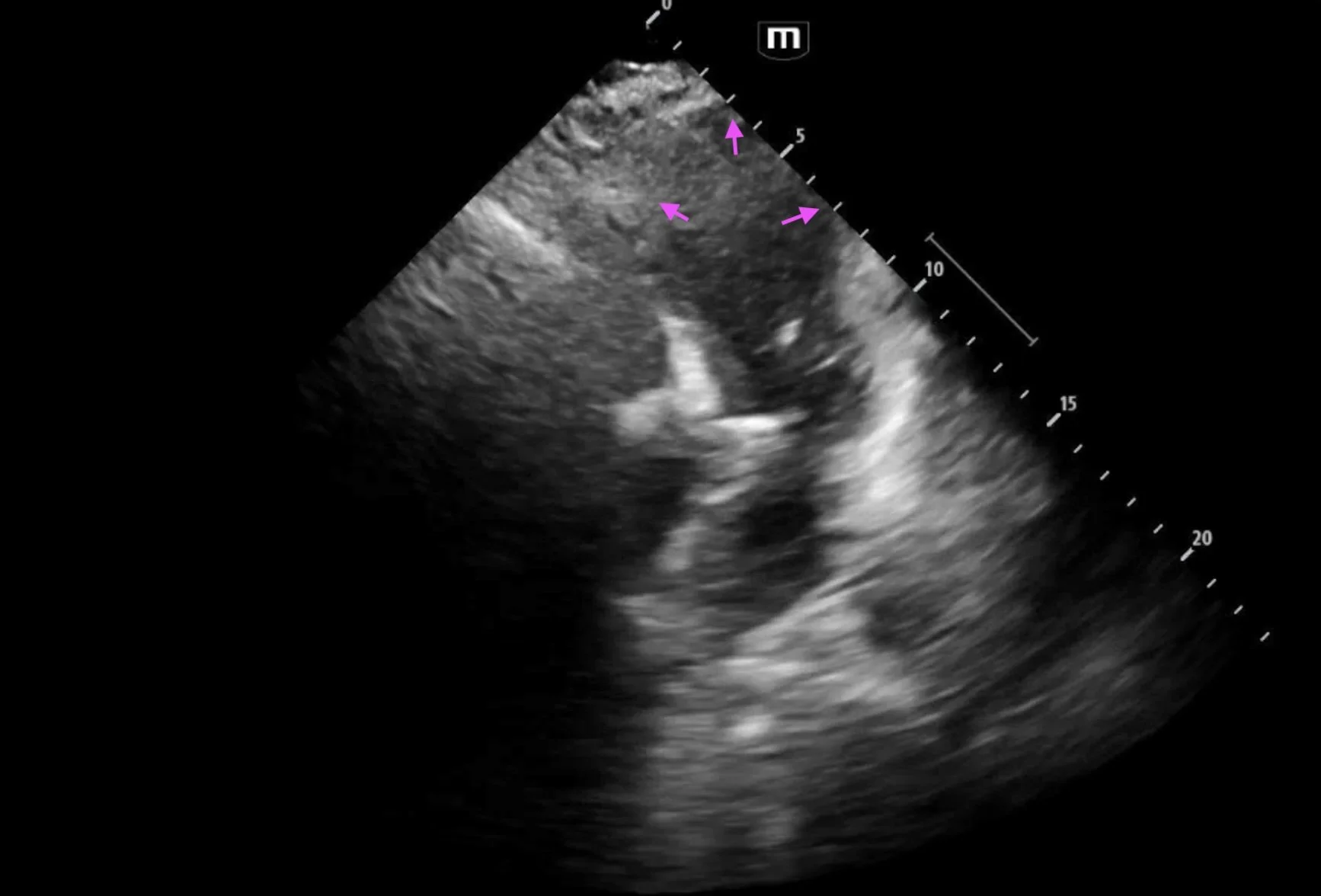
In this episode, Nick is being prepared for a confirmatory study, which is usually only indicated if prior studies are inadequate or if mimics like locked-in syndrome are suspected. The study of choice is cerebral scintigraphy, what Dr. Robby refers to as a "cerebral perfusion study": radiolabeled dye (technetium) is injected, and uptake into the brain tissue is evaluated based on presence of dye. In brain death, there is no uptake into brain tissue. As Dr. Robby warns the parents, this is the final test.
For NY specifically, the NYS Department of Health uses the 2023 consensus guidelines by the American Academy of Neurology. They include an excellent flowchart that can be used to guide one down the pathway of brain death testing. In short, the first considerations are whether a disease process causing brain damage has occurred, if other reversible causes have been excluded or corrected, if sufficient time has passed to establish permanency (recommending 48 hours for < 2 months of age, 24 hours for > 2 months of age), and if there are no signs of brain function at or above the level of the brainstem based on exam. Following an exam indicative of total loss of such brain function, the next step is apnea testing vs ancillary tests (EEG, 4-vessel catheter angiography, radionuclide perfusion scintigraphy, transcranial doppler if adult). One definitive apnea test or ancillary test in adults is enough to declare brain death; for pediatric patients, the recommendation is for a 2nd round of testing after a 12-hour observation period.
I want to also briefly mention a third "type" of death that isn't so much medical as philosophical. One could use the phrase ego death, or personality death — the loss of one's identity and personhood. The human experience encompasses more than what our meat alone would indicate, and defining "death" based solely on the activity of said meat can sometimes feel crude. The concept of ego/personality death is one approach to the question of "at what point of dysfunction do I stop being myself?" I.e., as your mind loses function, at what point would you consider yourself to be gone? This can be useful to consider when determining your own goals of care.
Other little lessons from episode 4:
Dr. Robby teaches us about Ho’oponopono, a Hawaiian prayer of healing and reconciliation. He specifies 4 phrases "that matter most": “I love you. Thank you. I forgive you. Please forgive me.”
Lower abdominal pain (that may be cyclical) in a "premenarchal" young female should prompt consideration of imperforate hymen. Please handle the conversation more delicately than Dr. King.
Starting BiPAP on a patient with a pneumothorax will lead to tension pneumothorax. I'm convinced that Dr. Santos did it maliciously, so as to create a need for a chest tube, a procedure that she had been itching to perform. More broadly, as a trainee, please update your supervisors about interventions you want to perform, especially on your first day.
Betting on ambulance chases should not be done in view of patient care areas.
References:
https://pmc.ncbi.nlm.nih.gov/articles/PMC3372912/
https://www.uptodate.com/contents/diagnosis-of-brain-death
https://www.uptodate.com/contents/evaluation-of-the-potential-deceased-organ-donor-adult
https://emcrit.org/ibcc/brain-death/
https://jnm.snmjournals.org/content/44/5/846
https://www.health.ny.gov/professionals/hospital_administrator/determining_brain_death/docs/aan_brain_death_guidelines.pdf