It's Friday, and time for our #3 installment of "Lessons Learned from the Pitt"!
No real spoilers today.
In the previous episodes, multiple rats were released into the ED from an undomiciled man's jacket. The status of the rat hunt continues in the background throughout the episode, with Dr. Collins at one point citing that the rats constitute a health risk to the patients. Given that we live in a decaying city that is thoroughly infested with all sorts of vermin, including the infamous "toilet rats", I thought I'd talk briefly about murine-associated diseases and their presentations.
Mice and rats have plagued humanity since the era before the written word, and as such are a significant reservoir of zoonotic diseases. Diseases can be spread by direct contact (including bites/scratches), by parasites carried on the rodents, by inhalation/ingestion of fur or droppings, etc.
The most famous of the rodent-borne diseases is probably the plague. According to the CDC, there are 7 cases of plague in the US each year, usually in northern New Mexico and Arizona. 3,248 cases were reported in 2010-2015, with most occurring in rural villages of sub-Saharan Africa. The "Black Death" of the mid-14th century killed as many as half of the European population, and led to supply chain disruptions and labor shortages that significantly altered the sociopolitical landscape. Plague has also been used as a biological weapon in the past, such as the Mongols catapulting plague-ridden corpses into besieged cities, or the Imperial Japanese Army spreading plague in Asia while carrying out research/crimes against humanity on Chinese and Korean civilians (for which post-war prosecution was deliberately incompetent or conciliatory). The plague is caused by Yersinia pestis, a gram-negative anaerobic coccobacillus that is most commonly carried by Rattus rattus and Rattus norvegicus, with a flea serving as the vector between them and humans. Transmission may also occur through direct contact through mucosa or broken skin, or inhalation.
The most common manifestation of the plague is the bubonic plague, wherein Y. pestis proliferates through the lymphatic system and causes a marked and extremely painful lymphadenitis. Other than localized effects, the bacteria also produces toxins which lead to systemic inflammation. Septicemic plague develops as the bacteria proliferate in the blood, either secondary to the bubonic type or independently after direct transmission i.e. a flea bite; this type can cause disseminated intravascular coagulation, leading to peripheral necrosis and later gangrene. The inhalation of airborne droplets containing Y. pestis can cause pneumonic plague (along with spread from bubonic or septicemic types), which is essentially a rapidly-progressive severe pneumonia often associated with hemoptysis. If symptoms of septicemic or pneumonic plague develop, the disease is usually fatal without treatment.
Diagnosis is made based on clinical suspicion (generally, buboes and pertinent history) and confirmation is by culture and PCR. The CDC has provided some excellent tables of recommendations of antibiotic selection (linked in references below); in general, a fluoroquinolone or aminoglycoside is preferred for septicemic and pneumonic plague, with doxycycline also being a first-line option for bubonic plague. Post-exposure prophylaxis should be given to those with high risk exposure, whereas pre-exposure prophylaxis can be deferred if PPE is available for droplet precautions. Vaccination is of questionable efficacy, and the CDC does not recommend vaccination for travelers going to regions where plague has been endemic.
Next, a few other highlighted murine-associated diseases:
Leptospirosis
A very common zoonotic infection, spread by contact with soil/water contaminated by urine of not only mice and rats, but a wide range of domestic and wild animals. Initial symptoms are nonspecific and may mimic viral gastroenteritis, disease can progress to kidney injury, liver injury, coagulopathy, and meningitis. Laboratory testing requires special culture media or fly-out studies. Thankfully, the bacterium is susceptible to most beta-lactams and doxycycline, and will succumb to the usual broad-spectrum cocktail.
Murine Typhus
Another rickettsial disease, but the vector is fleas rather than ticks. Most patients will not recall any exposure. Symptoms are nonspecific, resembling a viral syndrome +/- a scattered maculopapular rash. This clinical syndrome often prompts us to give doxycycline which is effective and prevents further complications such as ARDS and seizures.
Hantavirus
Specifically name-dropped in the show (or in commentary?), this is a family of viruses that causes two major syndromes. Hantavirus pulmonary syndrome is the predominant type in the US, while hemorrhagic fever with renal syndrome was previously limited to Eurasia but has been brought to the US. The names are self-explanatory, with cytokine storm being the major contributor to severe symptoms. Supportive care (including ECMO) is the mainstay, and mortality is as high as 50-70% in these syndromes. 864 cases were reported in the US from 1993-2022, with 35% mortality.
Other little lessons from Episode 3:
CPR coaching is an important role during a cardiac arrest. Especially if your medical student is visibly tiring after multiple rounds of inadequate chest compressions.
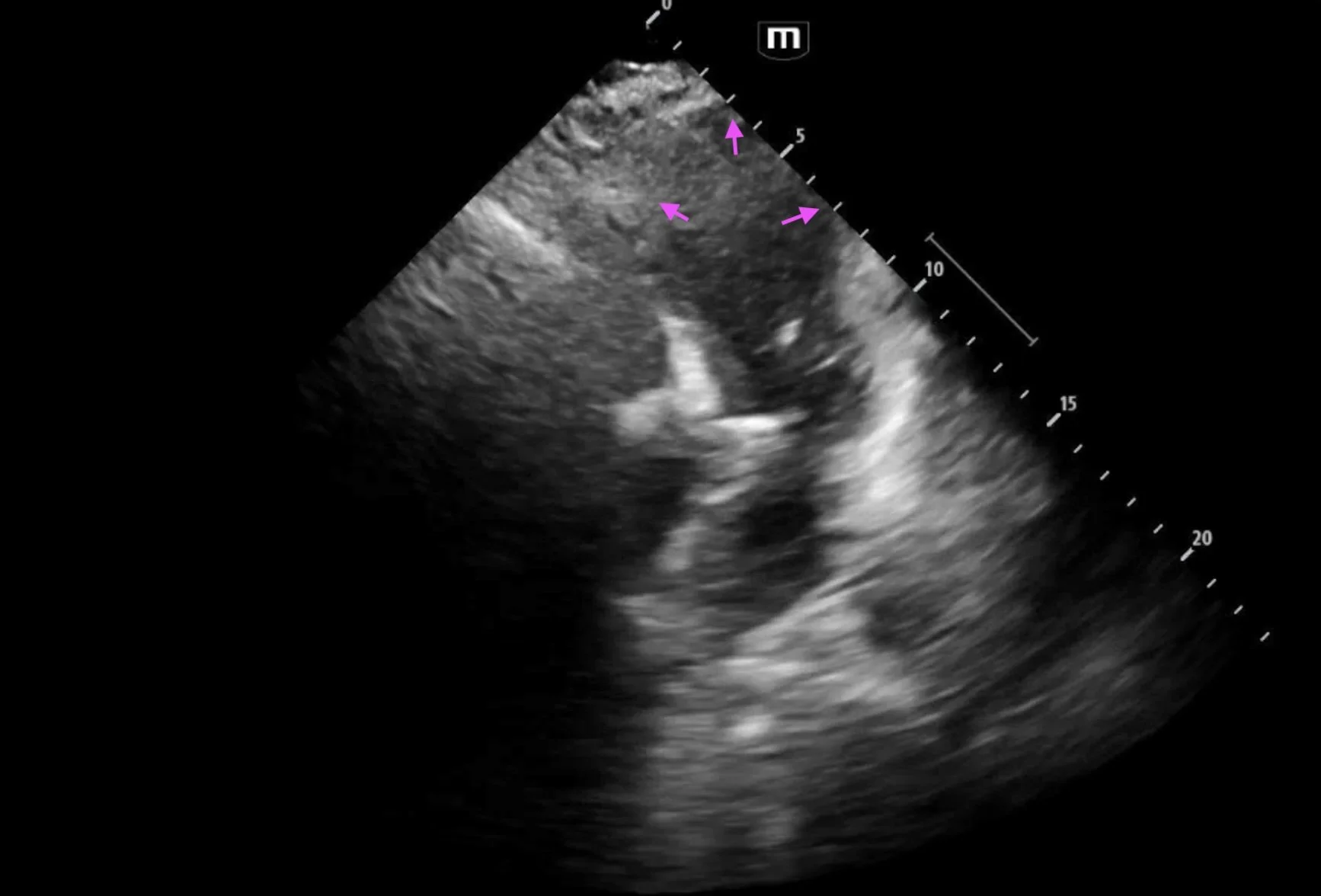
Deliberate right mainstem intubation can allow more "room to work" within the left side of the chest (as seen in the thoracotomy).
Profanity is not actually a sign of intelligence.
To the residents: if you're "comfortable", push yourself some more. This is your time to learn.
Visitor control is important in the ED. Our policy is 1 visitor per patient. Always confirm identity and patient's assent before sharing patient information.
References:
https://www.cdc.gov/healthy-pets/rodent-control/index.html
https://www.ncbi.nlm.nih.gov/books/NBK549855/
https://www.cdc.gov/plague/maps-statistics/
https://pmc.ncbi.nlm.nih.gov/articles/PMC8312557/
https://www.afro.who.int/media-centre/infographics/plague
https://www.ncbi.nlm.nih.gov/books/NBK441858/
https://www.ncbi.nlm.nih.gov/books/NBK513243/