Todays POTD will be a trauma topic we frequently talked about at Shock Trauma but less frequently at Maimo.
Blunt Cerebrovascular injury (BCVI): refers to a spectrum of injuries to the cervical carotid and vertebral arteries secondary to blunt trauma.
Why is this Important?
If left untreated, patients with BCVI are at increased risk for stroke. Mortality may reach as high as 43%. Rare diagnosis which makes it even more important to consider evaluating for in all of your trauma patients that meet criteria and have the associated risk factors .
Pathology:
The injury is caused by longitudinal stretching and injury to the vessels. Acceleration and deceleration can cause rotation and hyperextension of the neck, stressing the craniocervical vessels. This will lead to disruption of the intima. The intima tear then becomes a source of platelet aggregation that has a potential to cause downstream effects such as an embolic stroke or vessel occlusion
Risk Factors:
· High energy transfer mechanisms
· LeFort II or III fractures
· Mandibular fractures
· Complex skull fracture/basilar skull fracture/occipital condyle fracture (most common risk facture)
· Closed head injury with GCS < 6
· Cervical spine fracture, subluxation, or ligamentous injury at any level
· Near hanging with anoxic brain injury
· Clothesline type injury or seat belt abrasion with significant swelling, pain, or AMS
· Traumatic brain injury with thoracic injuries
· Scalp degloving
· Blunt cardiac rupture
· Upper rib fractures
Signs/Symptoms:
· Arterial hemorrhage from neck/nose/mouth
· Cervical bruit in patient < 50 years old
· Expanding cervical hematoma
· Focal neurologic defect
· Neurologic defect inconsistent with CT head findings
· Stroke on CT or MRI
Diagnostics:
· Standard of care CTA (80% sensitive and 97% specific)
Should be considered when patient has one or more of the risk factors or signs and symptoms
· Can also do MRI or arteriography but this is time consuming and labor intensive
Grading Scale:
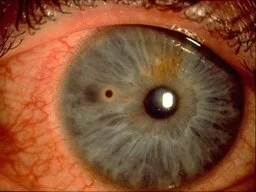
1. Grade 1: Intimal irregularity or dissection < 25 % of luminal narrowing noted
2. Grade 2: Dissection or intraluminal hematoma with > 25% luminal narrowing, intraluminal clot or visible intimal flap
3. Grade 3: Pseudoaneurysm
4. Grade 4: Complete occlusion
5. Grade 5: Transection with active extravasation
Management:
· Antithrombotics (heparin) or Antiplatelets (aspirin, Plavix)
· Operative repair
· Endovascular stenting
· Grade 1 and 2 injuries: single antiplatlet agent (aspirin 81 or 325mg)
· Grade 3: dual antiplatelets or therapeutic anticoagulation (heparin drip with PTT at goal)
· Grade 4 and above: Dual antiplatelets or therapeutic anticoagulation as well as operative or endovascular intervention
· Many low grade injuries heal within 7-10 days therefore early repeat CTA is recommended. Otherwise treatment may need to be continued for 3-6 months.
References:
· https://www.emra.org/emresident/article/blunt-cerebrovascular-injury/
· https://rebelem.com/blunt-cerebrovascular-injury-bcvi-universal-imaging-for-all/
· https://jss.amegroups.com/article/view/3790/html
· https://radiopaedia.org/articles/blunt-cerebrovascular-injury?lang=us
· https://www.aliem.com/guideline-review-east-blunt-cerebrovascular-injury/