Today we will show you how to actually measure HU on our radiology software, Medview/ PACS.
First open the CT and find the slice where you would like to measure the HU of a particular area. In the first image below, we see some free fluid around the liver which we would like to know whether it is blood or ascites.
Follow the steps in the images below and your HU measurement is on the second line. In this case, the free fluid in this patient's abdomen had a HU of 19.5 which is consistent with ascites.
Stay well,
TR Adam
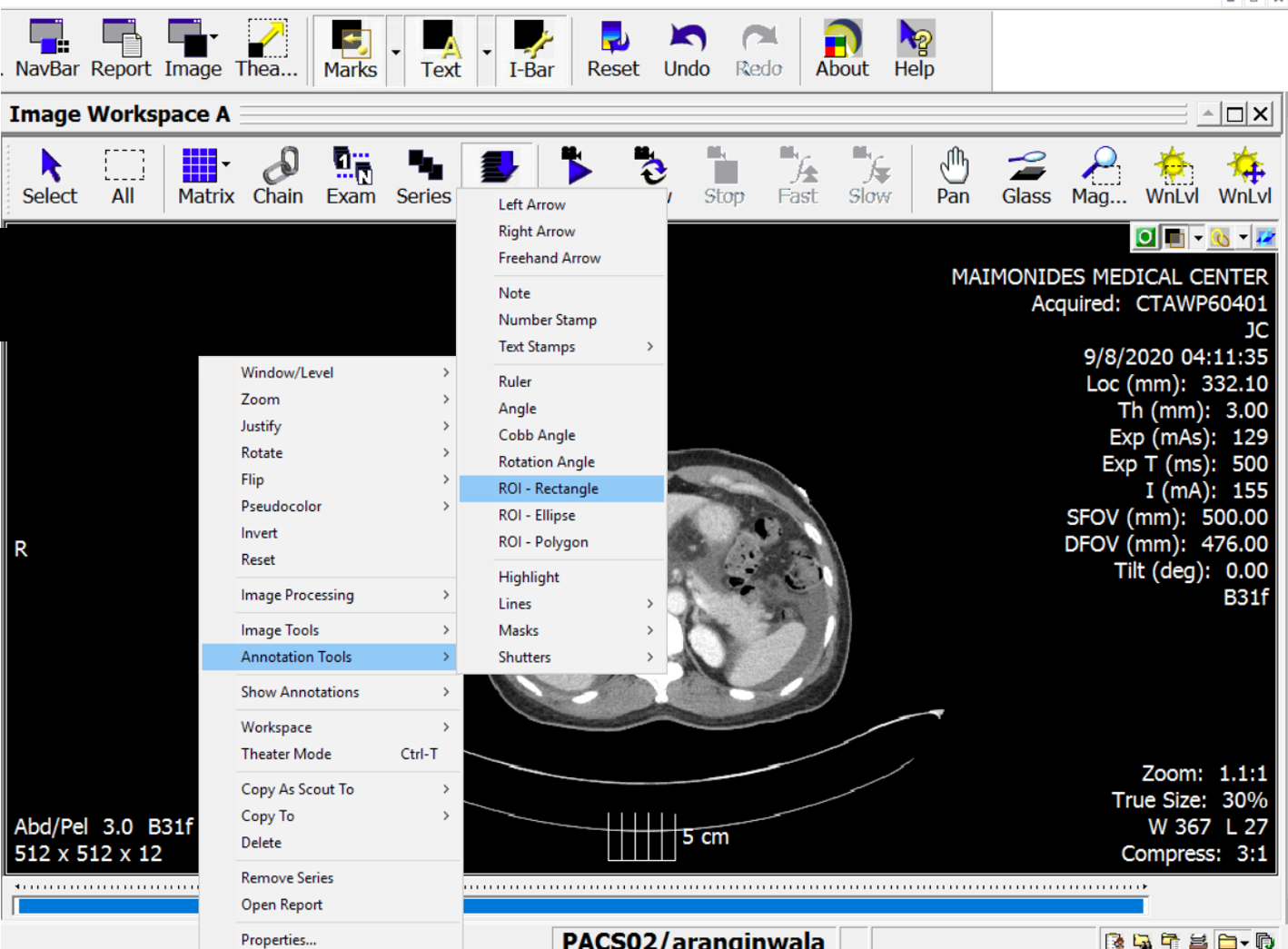
Right click on the image to open the following menu bar
Go to "Annotation Tools" on the menu bar and find and click on "ROI- Rectangle:"
Now create a small box (drag your mouse) over the area you would like the measure the HU. Make sure not to overlap over another area of the slice or it will distort your measurement. You may want to magnify the area you would like to measure