Welcome back to POTD.
The weekend has come and the weekend has gone. I know you've all been holding your breath to hear about----
A message from our sponsors:
Take a deep inhale. feel some wellness. feel the firmness of your feet on the floor. hold onto your seat.
Exhale nice and slowly......like someone with a COPD exacerbation.
Because today we're discussing antibiotic coverage in acute COPD Exacerbations. I know you've been waiting a lung time for this one.
Background
Acute COPD exacerbations (AECOPD) account for ~1.5 million ED visits annually in the ED.
Many physicians routinely prescribe antibiotic coverage for AECOPD
a 2018 review demonstrated antibiotic prescriptions given on 39% of ED visits for AECOPD between 2009-2014.
Due to the structural changes in the bronchi of COPD patients they are more prone to bacterial colonization (as opposed to asthmatics - which have no structural change but a reactive process)
Do guidelines exist?
Sure do.
if the patient appears infectious (think fever) administer antibiotics. This is understandable given their risk factors and bronchial structural changes.
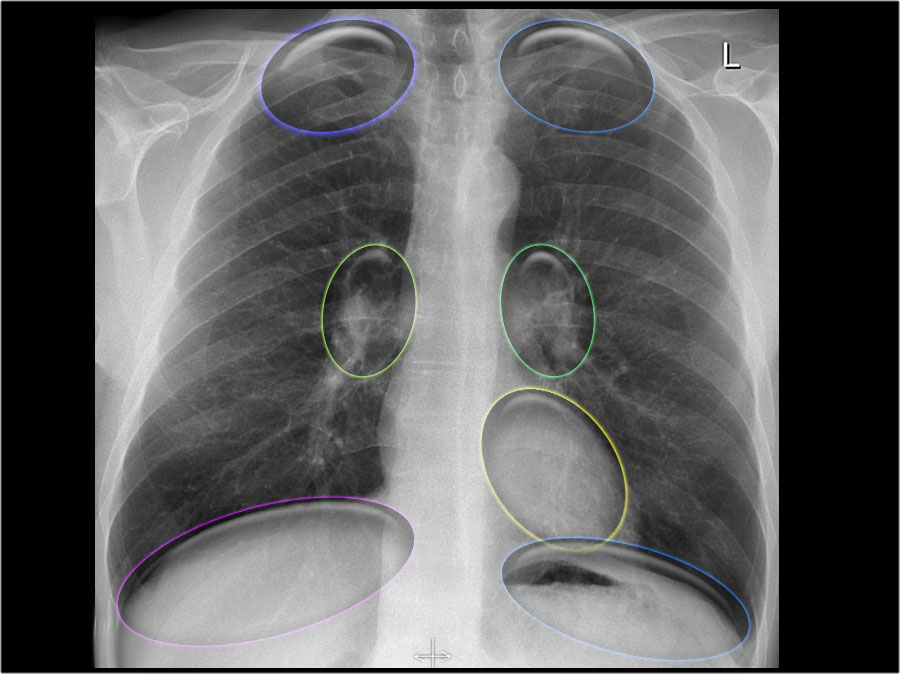
Several guidelines exist for more subtle cases, they exist as follows: (see chart below)
Global initiative for Chronic Obstructive Lung Disease:
Antibiotics should be given to
patients with all 3 of the following cardinal symptom
increased dyspnea
increased sputum volume
increased sputum purulence
patients with 2 cardinal symptoms, if there is increased purulence
patients requiring noninvasive or invasive ventilation
American Thoracic Society/European Respiratory Society
hospitalized patients with chanegs in sputum characteristics
all patients admitted to an ICU
Canadian Thoracic Society
patients with severe purulent AECOPD
National Institute for Health and Clinical Excellence
patients with more purulent sputum
Basically, pay attention to that sputum. take a thorough history and discuss changes in sputum production.
-Elly