POTD: Felon
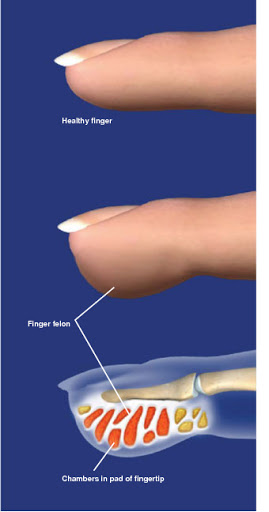
Subcutaneous pyogenic infection of the pulp space compartment of the distal finger
Can often be confused with paronychia or herpetic whitlow (fingertip pain but should not cause taut erythema) which can sometimes present with volar erythema
High risk to progress to osteomyelitis, Flexor Tenosynovitis!
Clinical Features:
Erythematous, edematous, tense distal pulp space with significant pain and tenderness
May see necrotic appearing tissue distally due to increased pressure in space
Work Up:
Usually diagnosed clinically
XR: No foreign body, soft tissue swelling pulp of thumb
US: Use the water bath technique to see a potential fluid collection
Digital Nerve Block
I & D is the cornerstone of management:
Apply a latex glove finger tourniquet
If the felon is on patient’s index, middle or ring finger, make the incision of the ulnar aspect
If the felon is on patient’s thumb or pinky, make the incision of the radial aspect
Using your #11 blade start your incision 5mm distal to flexor DIP crease and end 5mm proximal to nail plate border. Digital arteries and nerves arborize near DIT. Avoid those!
Blunt dissect and break any loculations until the abscess is decompressed
Avoid the "fishmouth" incision. Potentially can cause an unstable finger pad, neuroma or loss of sensation
Antibiotics: Cover for Staph (MRSA) and strep
Disposition:
Home with follow up in the hand clinic or ED in 1-2 days.
Check out this video to see it done:
Stay well,
TR Adam
Hello, World!