HPI: 42 yo male with no PMH presenting for abdominal pain x 2 days. His physical exam was significant for LLQ tenderness with guarding and rebound.
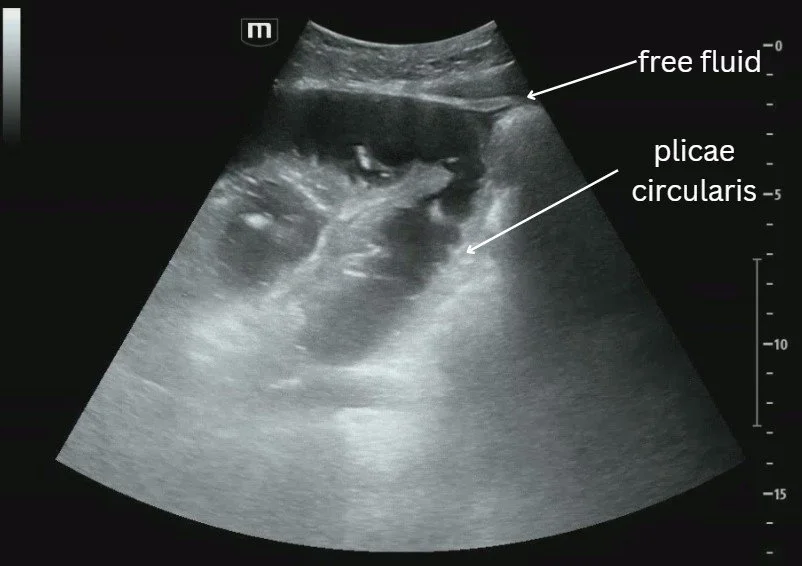
POCUS showed (see video):
We initially thought the outpouching connected to the abscess was a diverticulum but on further review, it’s more likely to be a loop of bowel given its size.
What a diverticulum should look like:
CT scan for reference:
Diagnosing Diverticulitis on POCUS
Use curvilinear vs linear probe
Start at maximal point of pain > lawnmower technique
#1: Find diverticula
Looks like outpouching attached to loop of bowel
Secondary findings:
Bowel wall diameter >5 mm
Prominent, fluid-filled bowel loops
Pericolic fluid collections
Increased pericolic fat (hyperechoic fat anterior to diverticula)
Intraabdominal abscesses
Case conclusion: CTAP showed perforated diverticulitis with multiple intraabdominal abscess. Patient was taken for IR drainage with feculent/purulent drainage noted. Patient is still doing well on surgical service.
References
https://www.ultrasoundcases.info/diverticulosis---diverticulitis-531/