Do you see what eye see?
Eye complaints can be abundant in the ED - so what should we focus on? Today's pearl is going to focus on the diagnoses of atraumatic vision loss.
Let's break it down by symptoms: Painless or painful?
Good physical exam must include: visual acuity, visual fields, pupillary exam, fluorescein woods lamp, slit lamp and of course - a head to toe complete physical exam.
Painless Vision Loss:
TIA/stroke: sudden vision loss usually from embolic or thrombotic event, can often be from carotid artery occlusion. If transient, often called amaurosis fugax but that can apply to any cause of transient vision loss. Risk factors: it is a stroke/TIA of the eye, so same cardiovascular risk factors. Testing: MRI, ECG, Echo, Carotid US. ED role: Don't miss it - this is a stroke and should admitted to a monitored stroke unit.
2. Central retinal artery occlusion: Sudden, permanent typically unilateral vision loss (permanent damage ~90 minutes of occlusion). Risk factors: atherosclerosisdisease (HTN, DM, Smoking, etc.) and treatment involves treating risk factors (varied success with laser treatment of pressure decreasing eye drops); or secondary to Giant cell arteritis (+/- headache, pain with hair burshing or chewing) in which case rapid high dose corticosteroids can prevent vision loss. PE: decreased visual acuity, asymmetric red reflex, "Cherry red spot" on the macula on fundoscopy. ED role: urgent/emergent optho referral or ED consult. Recognize if cause is giant cell arteritis (CRP, ESR) and treat with high dose steroids. Consider timolol 0.5% topical drops but no strong evidence. Will need PCP to address concurrent risk factors.
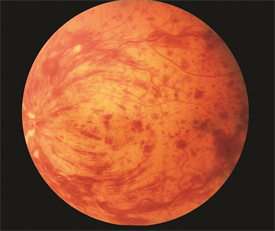
3. Central retinal vein occlusion: often times sudden but occasional gradual (days-weeks) vision loss due to swelling of the macula. Risk factors: same as above and glaucoma. Think of this as a DVT for the eye. PE: decreased visual acuity. "Blood and thunder" on fundoscopy. ED role: Evaluate for cause or presence of other pathologies secondary to a hypercoagulable state (DVT, PE, sickle cell, etc.). Refer to optho and will need PCP to address concurrent risk factors.
4. Retinal Detachment: Sudden, spontaneous "flasher and floaters" or "spots or stars" or loss of vision that is like a "curtain closing." Usually loss of peripheral vision. Risk factors: recent eye injury or surgery, severe nearsightedness (think elderly). ED Role: POCUS - look for a delicate floating line in the anechoic eyeball space. If their is no macular separation, their vision can be saved! This is an optho emergency. Unless you're Errel, err on the side of caution and call optho for all of these since we might not be able to definitively determine if the macula is involved.
5. Vitreous Hemorrhage and Posterior Vitreous Detachment: Floaters, strings, or cobwebs in their vision that change with eye movement. Flashes of light. Risk factors: retinal damage (surgery, trauma, prior retinal tear), Diabetic Retinopathy, trauma, sickle. ED role: POCUS: swirling cloud-like opacity at moves with ocular movement and is not tethered to the optic disk or retina "washing machine sign". ED role: Avoid Anticoagulation, elevate head of bed, optho referral.
6. Optic Neuritis/papillitis: painless vision loss over hours to days, typically unilateral. +/- prior episodes. +/- other neuro symptoms. May worsen with eye movement. Risk factors: typically females 18-45, multiple sclerosis. Viral: mono, zoster, encephalitis, TB. Physical exam: decreased acuity, relative afferent pupil defect, often normal fundoscopy; requires complete neuro exam. ED role: MRI brain. Diagnose underlying cause. Often required admission for continued IV high dose steroids.
Painful Vision Loss:
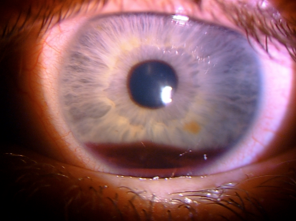
1. Acute angle glaucoma: sudden, usually form bright to dark environment (movie theater). Often with headache, N/V, and light sensitivity/halos. PE: midsize, nonreactive pupil. Must include tonometry, IOP>20! Risk factors: Asian, femaile, shallow anterior chamber. ED role: timolol 0.05% 1-2 drops (beta blocker, watch for systemic absorption SE) eye drops and brimonidine (alpha agonist) eye drops to reduce IOP. Miotic agent pilocarpine (2-4% 1-2 drops q15 m). Titrate until symptoms improve, IOP decreases. Systemic carbonic anhydrase inhibitors like acetazolamide 500 mg IV. Elevate head of bed. Treat nausea and headache, too! Urgent optho referral.
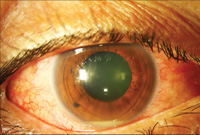
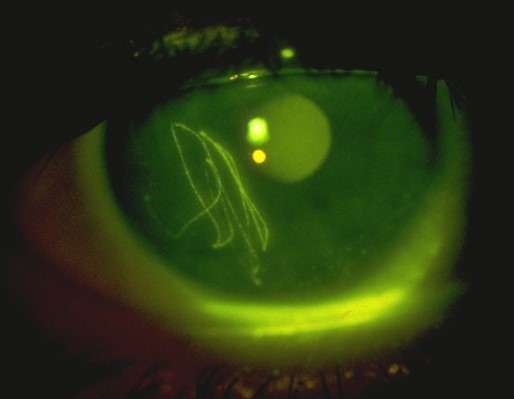
2. Corneal Ulcer: foreign body sensation, red eye. PE: injected conjunctiva, gray patch on cornea. Increased fluorescein uptake on Woods lamp. Possible hypopyon purulent collection. ED role: Evaluate for foreign body. Consider HSV keratitis. Start opthalmic antibiotic drops, must have pseudomonas coverage for contact lens wearers (tobramycin), consider antifungal. **Admit for IV ceftriaxone for suspected gonococcal infection. Will need optho evaluation and ulcer culture.
3. Uveitis/Iritis: painful, progressing red eye worse with eye movement, +photophobia suggests anterior. Floaters suggests posterior, often no pain. Can be panuveitis. Causes can be inflammatory (HLA B-27 usually bilateral, eg. reactive arthritic, psoriasis, IBD, ankylosing spondylitis; sarcoid, Kawasaki), traumatic, infectious (toxoplasmosis, CMV, HSV, adeno, measles, mumps, TB, syphilis, Lyme), or secondary to medications(sulfa). PE: injected conjunctiva with ciliary flush (erythema around the iris). Sluggish, constricted, or irregular pupils. Slit lamp shows cloudy anterior chamber and "cell and flare." ED role: evaluate for underlying cause (STD screen, CXR for TB, etc.) and refer to optho urgently and appropriate f/u.
I am certain that this is not a comprehensive list, so please - learn on!
Buzzword pearls to part with:
Life in the Fast Lane has some great blogs for symptom/disease specific presentations with pictures: https://lifeinthefastlane.com/resources-for-ocular-emergencies/ and Steve Carroll's EM Basic’s eye complaint sheet is incredibly useful as well.
Happy Learning!
References:
https://www.merckmanuals.com/home/eye-disorders/symptoms-of-eye-disorders/vision-loss,-sudden
https://www.acepnow.com/article/essential-ophthalmologic-procedures-and-exams-for-the-emergency-department/
https://www.asrs.org/patients/retinal-diseases/22/central-retinal-vein-occlusion
https://litfl.com/a-man-of-singular-vision/
https://litfl.com/flashing-and-floating/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4170392/