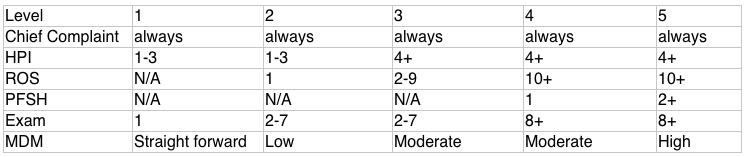
Let's break down a chart and assign meaning to the table above:
Chief Complaint:
Always include this no matter what
Typically the main reason the patient states when you ask them what brings them to the ER
HPI:
In the table above, this refers to how many elements of the chief complaint need to be in this section.
For example, a patient coming in for simple suture removal, this would be a level 1 chart, and you may include the location of the sutures as the 1 element.
For a patient coming in with chest pain, this is at least a level 3 chart, and should include at least 4 elements such as the location, onset, severity, and duration of the pain. This is just a minimum and you should include other elements as appropriate.
For a complaint that the patient has had for >72 hours, make sure to document why it necessitates emergency care. For example "patient's pain acutely worsening today" or "patient was unable to schedule outpatient appointment as all offices are closed due to COVID-19 pandemic."
ROS:
In the table above, this refers to how many systems need to be in this section.
For example, a patient coming in for simple suture removal, this would be a level 1 chart, and you really don't need anything in the ROS but you can at least include a problem-pertinent ROS such as the Skin system in case it's able to be billed as a level 2 chart.
The line in the template that states "All other systems negative" is placed there as a fail-safe because the ROS is typically a section that is not documented enough. By having that line there, it automatically allows the coders to bill at the highest level for this section but is medico-legally questionable if you only have a few systems there and then have that templated line.
Best practice for a level 3 chart and higher would be to truthfully document all 10 systems and as long as you have the 10, you don't actually need that templated line.
If you cannot obtain a ROS, you need to say why (e.g. patient is intoxicated, obtunded, in cardiac arrest).
PFSH:
In the table above, this refers to how many elements you need from past medical, family, and social history.
For example, a patient coming in for simple suture removal, this would be a level 1 chart, and you really don't need any information here.
This is the easiest section to make sure is complete because our smoking question is a requirement for you to fill out and that automatically gives you 1 element right there. You also typically always include PMH in your HPI and that would be your second element.
If you are using family history as one of your elements, you need to be specific. It's not enough to say that it is "non-contributory."
Exam:
In the table above, this refers to how many organ/body systems you need to include in this section.
For example, a patient coming in for simple suture removal, this would be a level 1 chart, and you can include your skin exam to satisfy this requirement.
MDM:
In the table above, this refers to the complexity of your decision making in the case.
This is one of the main sections that coders look at and is arguably the most important section of the chart.
Coders determine how complex the case is based on the information included in this section and they typically look at the number of differential diagnoses and problems that you are addressing, the amount and complexity of diagnostics you are ordering and your interpretation of them, and the risks of complications, morbidity/mortality for this patient.
This information can also be in your progress notes rather than in the MDM as information comes back and circumstances change while you are taking care of the patient.
As a side note, it's best to complete the chart in real-time and complete progress notes as you gather more information, results come back and you interpret them, you reassess your patient, etc.
Diagnosis:
List all the diagnoses addressed during the encounter. List the most severe ones first. Don't forget to include complaints and vital sign abnormalities.
For example a patient you are admitting with a PE could potentially have all the following diagnoses: pulmonary embolism, acute chest pain, shortness of breath, hypoxia, tachycardia, tachypnea
--------------------------------------------------------------------------------------------------------------------------------
It's difficult to know which level each chart will be billed at so always chart to a level higher if you are unsure.
Some examples of level determination factors to help guide you:
Level 1 chart
suture removal, insect bite, wound check, dressing change, med refill
no meds given in ED, no tests ordered
Level 2 chart
Level 3 chart
any imaging or blood work ordered automatically makes it at least a level 3
any medication given in the ED automatically makes it at least a level 3
simple procedure such as laceration repair
Level 4 chart
Level 5 chart
Common documentation omissions that result in downcoding:
1) In a trauma, it's not enough to write "MVA" or "Fall" for the diagnosis. If there are no acute injuries found, you still need to justify all of the imaging and workup ordered. If the patient came in complaining of left arm pain and you x-rayed the arm, include "left arm pain" in your list of diagnoses.
2) Filling out the procedure note for CPR. The nursing flowsheet is unfortunately not enough. A physician on the chart has to document the fact that CPR was performed.
3) Make sure to include what you did for fracture management, even if it's as simple as applying buddy tape, providing crutches, providing follow-up information.
4) Fully complete all elements in a procedure note. For example in a laceration repair, include length and depth of laceration and document if it was complex and you did any debridement.
For an abscess, a simple I&D pays about $100 but if it was loculated and you probe it to break up loculations and then document it as complex, that pays about $185!
In contrast, an intubation only pays about $150 and a PSA only pays about $13!
5) Don't forget to document your interpretation of vital signs, imaging, labs, ekg (must include reason for ekg and at least 3 elements such as rate and rhythm, axis, ST abnormalities, comparison to previous). This can be done in progress notes.
6) A lot of what we do falls into what is billable for critical care time but we often forget to document it. This includes speaking with family members about goals of care, speaking to consultants, speaking to primary care providers, reviewing old charts, obtaining IV access if the nurse is unable to do so.
For attendings, don't forget to chart your critical care statement!