by David Shang
Each EKG this week comes from a patient with chest pain. Answer the following questions for each EKG:
1) What are the concerning features?
2) Where’s the lesion?
3) Does this patient require cath lab?
EKG #1
EKG #2
EKG #3
EKG #4
EKG OF THE WEEK #6 Answers
This week was recognizing STEMI equivalents.
· While almost everyone can recognize STEMI on EKG (revisit Duncan’s examples of benign vs. scary STE), there are unfortunately many EKG patterns that are associated with coronary vessel occlusion.
While not an all-encompassing list, hopefully here are a few more patterns you can add (especially for my co-interns).
Besides possibly Wellen’s Syndrome (EKG #1), the other 3 EKG’s all demonstrate coronary artery stenosis that requires cardiac catheterization and reperfusion.
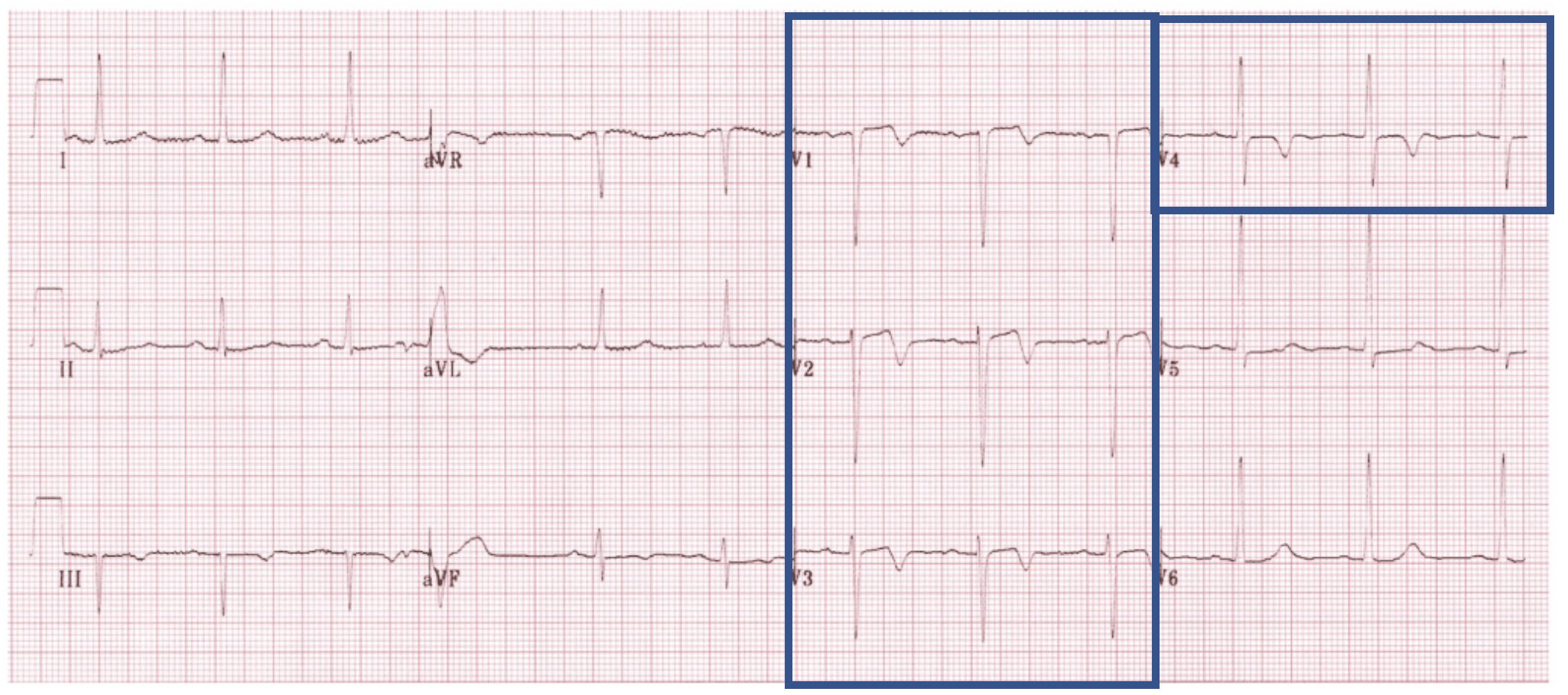
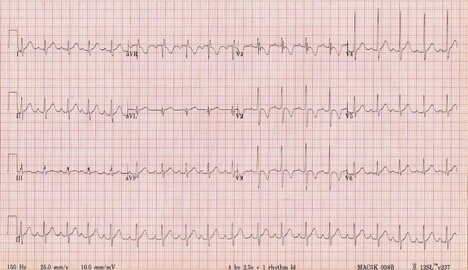
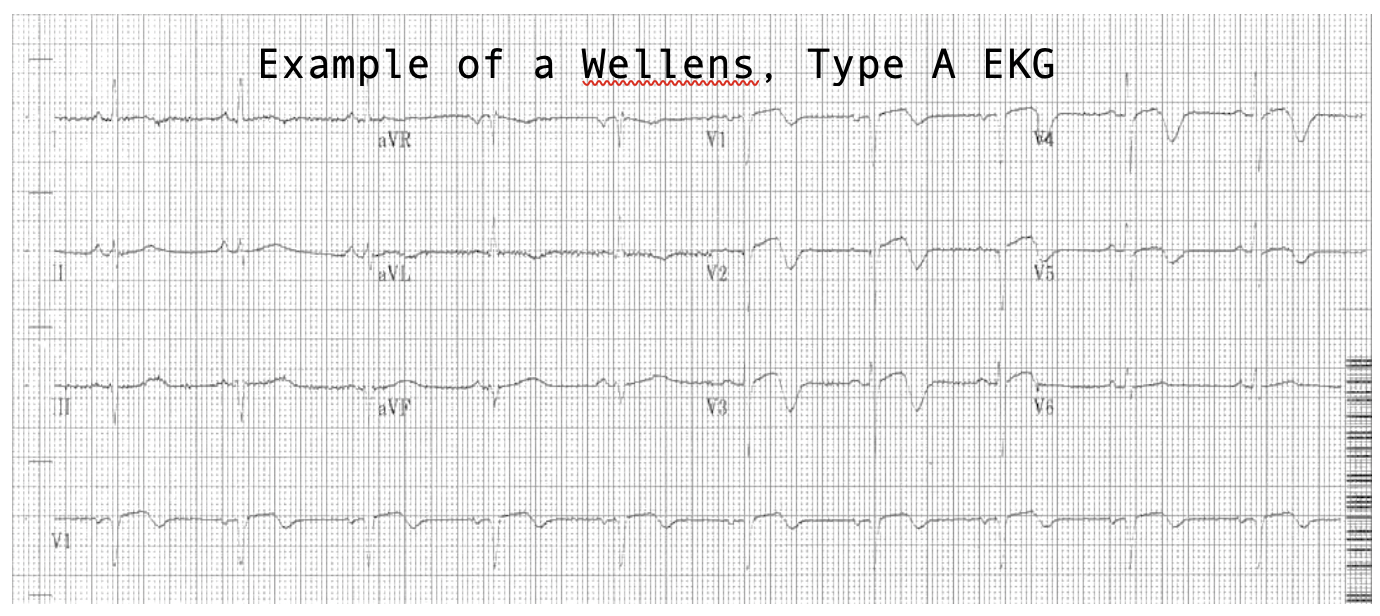
EKG #1: Wellen’s Syndrome Type A– Look at T-waves in V1-V4
- Associated with proximal high-grade LAD occlusion. According to REBELEM, Wellen’s waves + history of chest pain + normal/minimally elevated troponin = 86% PPV for LAD lesion
- Important to recognize that this pattern persists even if chest pain resolves. Refer to last week’s EKG for Duncan’s full explanation of the pathophys but…
o Believed to be a pattern of sudden occlusion + reperfusion. The T wave morphology is very similar to patients who reperfuse following successful PCI.
o Despite resolution of chest pain, patients remain at high risk of re-occlusion
- Two Types – both involve T-waves in the precordial leads (usually V2-V3)
- Requires cardiology consult but may not require immediate cardiac catheterization. However, if they do not go for cath requires antiplatelet and antithrombotic therapy as well as continuous 12-lead ST segment monitoring to detect any re-occlusions
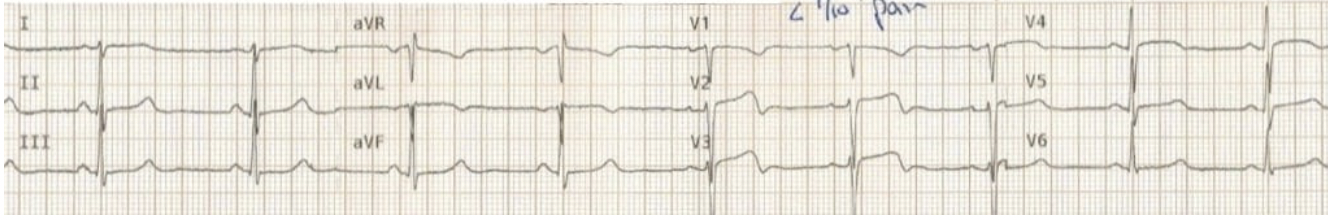
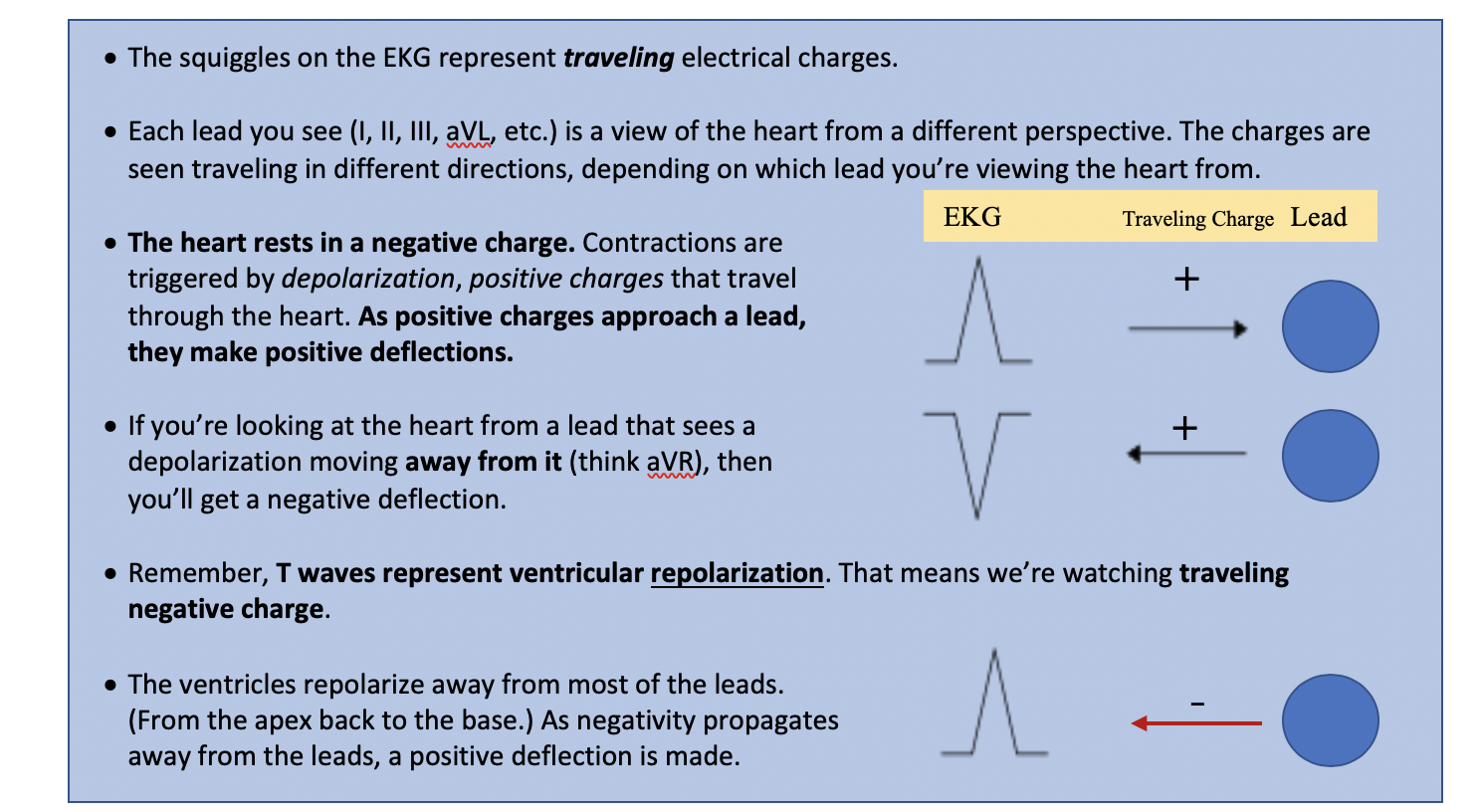
Finally, an example demonstrating the pattern of LAD occlusion, reperfusion, and re-occlusion. From LITFL, EKGs in chronological order over a 45 min period.
(a) Patient experiencing chest pain and diaphoresis
· The ECG shows a clear anterolateral STEMI, with inferior reciprocal change.
· The artery is occluded at this point.
(b) Resolution of pain
· The ECG now shows a typical Wellens pattern of biphasic T waves in V2-3, plus improvement in the anterolateral ST elevation.
· This indicates spontaneous reperfusion of the LAD — i.e. the artery has re-opened.
(c) Recurrence of chest pain and diaphoresis
· With recurrence of pain there is pseudo-normalisation of the precordial T waves: the previously biphasic T waves have become prominently upright (= “hyperacute” T waves).
· This apparent normalisation of the T waves indicates re-occlusion of the LAD artery.
Further reading: https://litfl.com/wellens-syndrome-ecg-library/
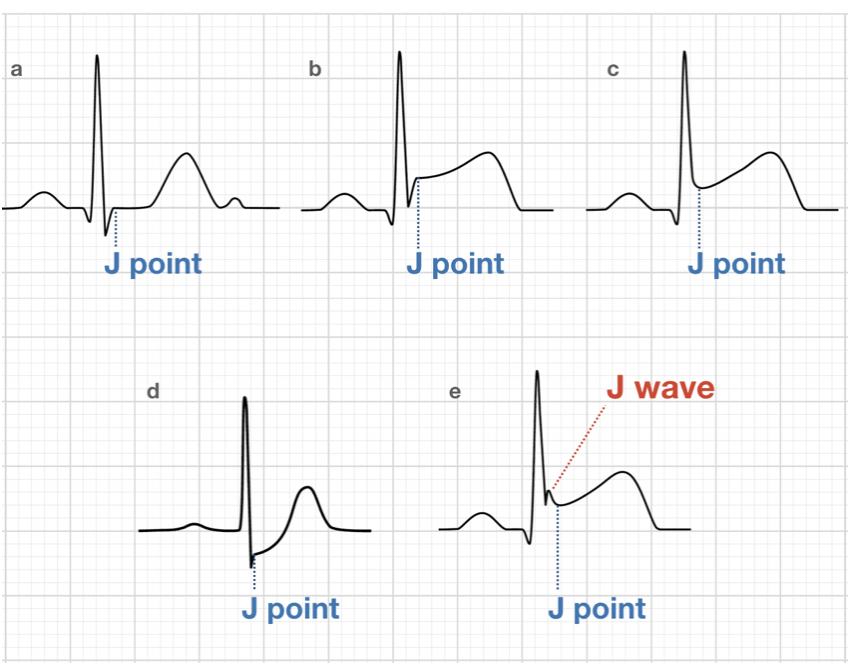
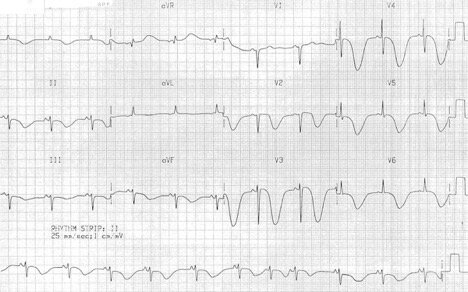
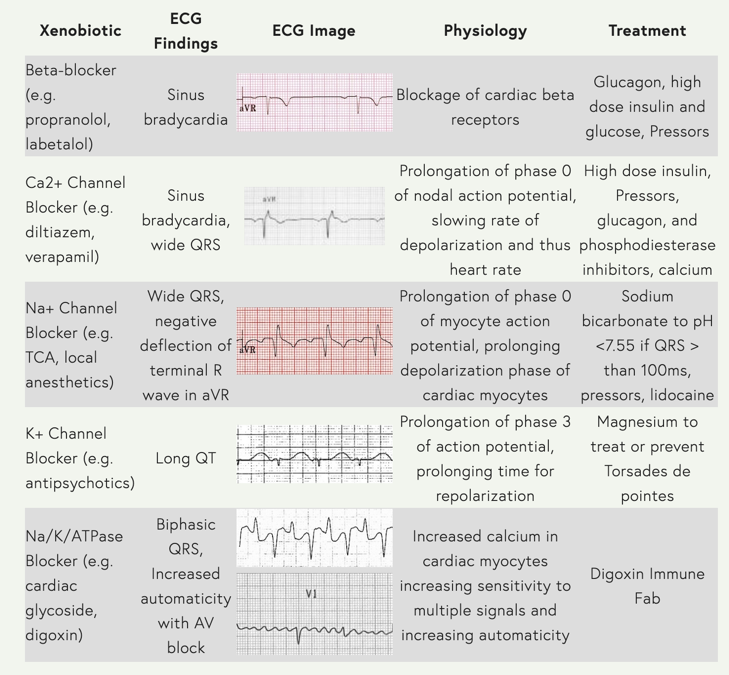
EKG #2: De Winter’s T Waves – Look at V1-V6, aVR +/- aVL
- Also associated with proximal LAD occlusion (pattern found in 2% of acute LAD occlusions)
- Anterior STEMI equivalent without obvious ST segment elevation
- Findings
o Leads V1-V4: Up-sloping ST depressions at J point
o Leads V1-V4: Tall, symmetric T-waves
o aVR +/- aVL: ST elevation
- This has features of both De Winter’s T waves and anterior STEMI
o ST elevations in V1-2, I, aVL with inferior reciprocal changes
o Upsloping ST depression and peaked T waves in V3-6
Further Reading: https://litfl.com/de-winter-t-wave-ecg-library/
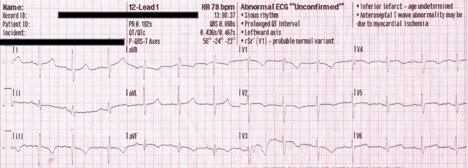
EKG #3: Posterior MI – look at leads V1-V3
- Accompanies 15-20% of STEMIs, usually occurring with inferior or lateral infarction. Posterior involvement implies a much larger area of myocardial damage
- Isolated posterior MI is less common (3-11% of infarcts). The lack of obvious ST elevation makes this more difficult to diagnose.
- Typical next step is to get posterior EKG with leads V7-V9
- Signs:
o Horizontal ST depression in V1-V3
o Tall, broad R waves (>30 ms)
o Upright T waves
From LITFL: The anteroseptal leads are directed from the anterior precordium towards the internal surface of the posterior myocardium. Because posterior electrical activity is recorded from the anterior side of the heart, the typical injury pattern of ST elevation and Q waves becomes inverted:
· ST elevation becomes ST depression
· Q waves become R waves
· Terminal T-wave inversion becomes an upright T wave
I see it as viewing the reciprocal change of a posterior STEMI through the anterior leads. I use the PAILS mnemonic (P-posterior A-anterior I-inferior L-lateral S-septal): ST elevations in one set of leads has reciprocal changes in the leads of the next letter.
- A posterior STEMI will have reciprocal changes in the anterior leads
Further Reading: https://litfl.com/posterior-myocardial-infarction-ecg-library/
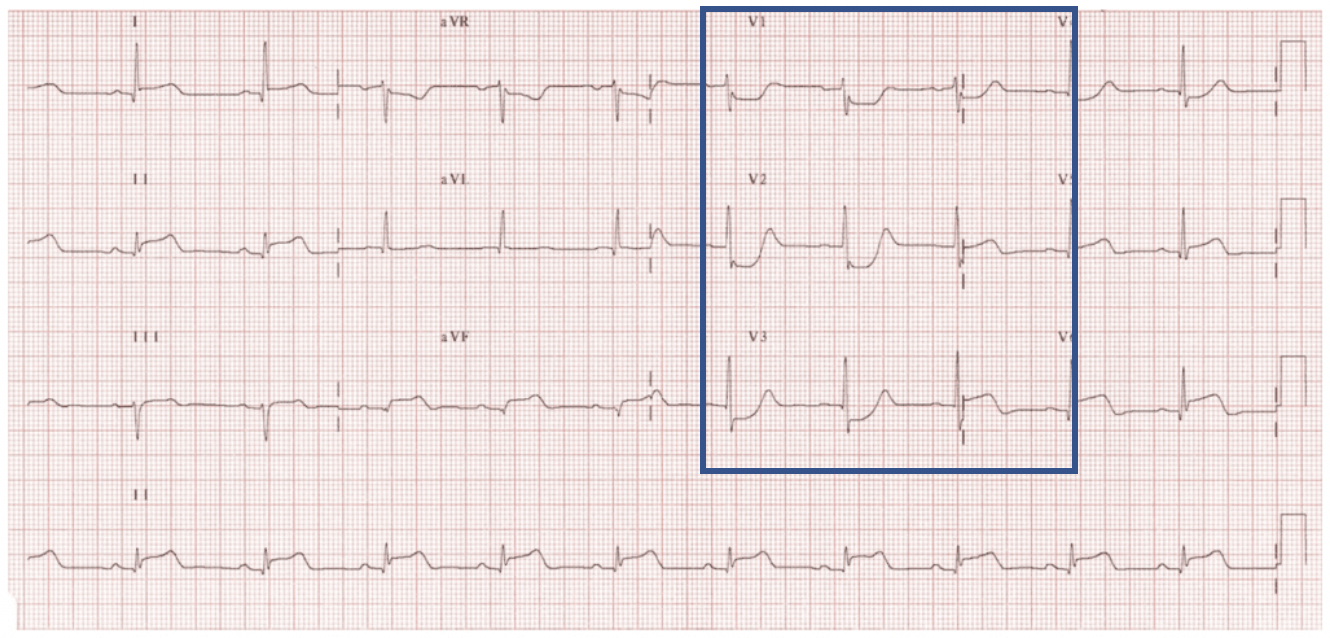
EKG #4: Left Main Coronary Stenosis – Look at aVR in particular
- No fancy name here - usually due to stenosis of Left Main Coronary Artery
o Semantic, but some argue that it be called “stenosis” because complete occlusion would result in STEMI, cardiogenic shock, and death
- Findings:
o Widespread ST depression, most prominent in leads I, II, V4-6
o ST elevation in aVR > 1mm
o ST elevation aVR > V1
ST Elevation in aVR also found in:
- Proximal LAD occlusion (remember it was also found in De Winter’s!)
- Severe triple-vessel disease
- Diffuse subendocardial ischemia
- Mechanism: LMCA stenosis causes subendocardial ischemia to the left side of the heart, resulting in diffuse ST depressions (especially in leads I, II, V4-6)
o aVR (representing the right side of the heart) is electrically opposite to the left sided leads à resulting in ST elevation in aVR
· STE in aVR ≥ 1mm indicates proximal LAD / LMCA occlusion or severe 3VD
· STE in aVR ≥ 1mm predicts the need for CABG
· STE in aVR ≥ V1 differentiates LMCA from proximal LAD occlusion
· Absence of ST elevation in aVR almost entirely excludes a significant LMCA lesion
· Marked ST elevation in aVR >> V1
· ST depression in mulitple leads (V2-6, I, II, aVL, aVF)
· This patient presented to ED in cardiogenic shock
NOT LMCA Stenosis!
· A septal STEMI, with ST elevation and Q wave formation in V1-2
· ST elevation in aVR = ST elevation in V1
· Widespread ST depression, most prominent in leads I, II and V5-6
Given the signs of septal STEMI, this ECG most likely represents a proximal LAD occlusion.
Further Reading: https://litfl.com/lmca-occlusion-st-elevation-in-avr/