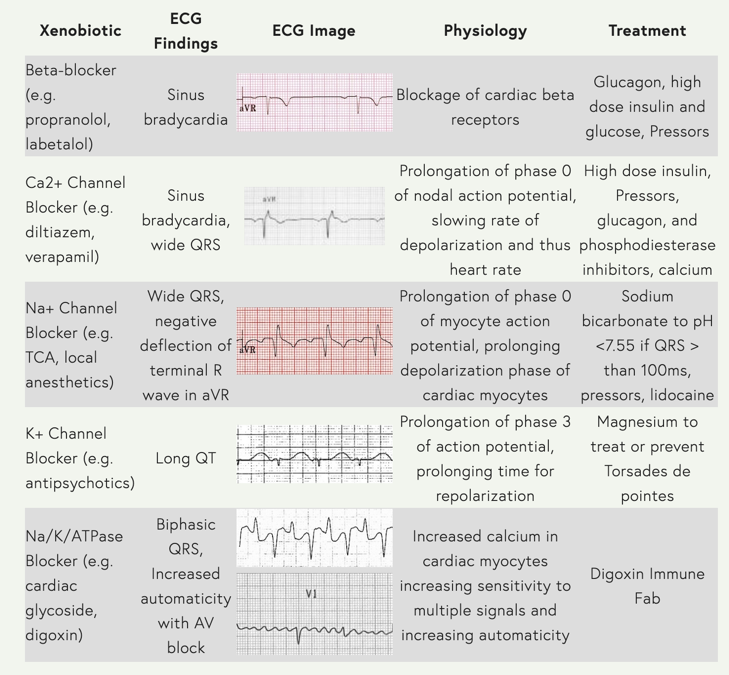
EKG#1
80 year old demented female, unresponsive, BP 55/20, blood glucose 24
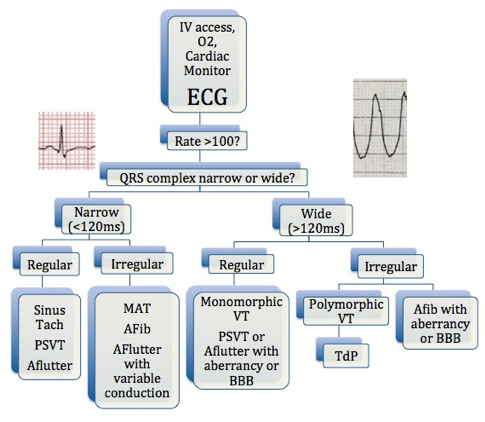
1. What’s the rhythm?
2. What’s the differential for bradycardia?
3. Think tox – now narrow your differential. What do the vitals suggest?
4. How do you want to treat this patient?
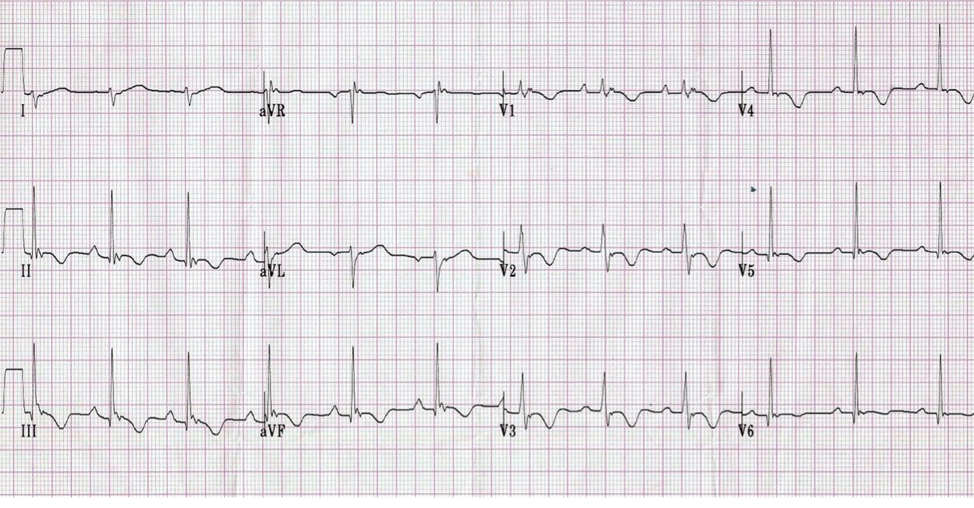
EKG#2
21 year old male, suicidal, intentional overdose
1. Rate, rhythm, axis, intervals – you can glean a lot of information from these pieces alone
2. What’s the suspected overdose?
3. Treatment?
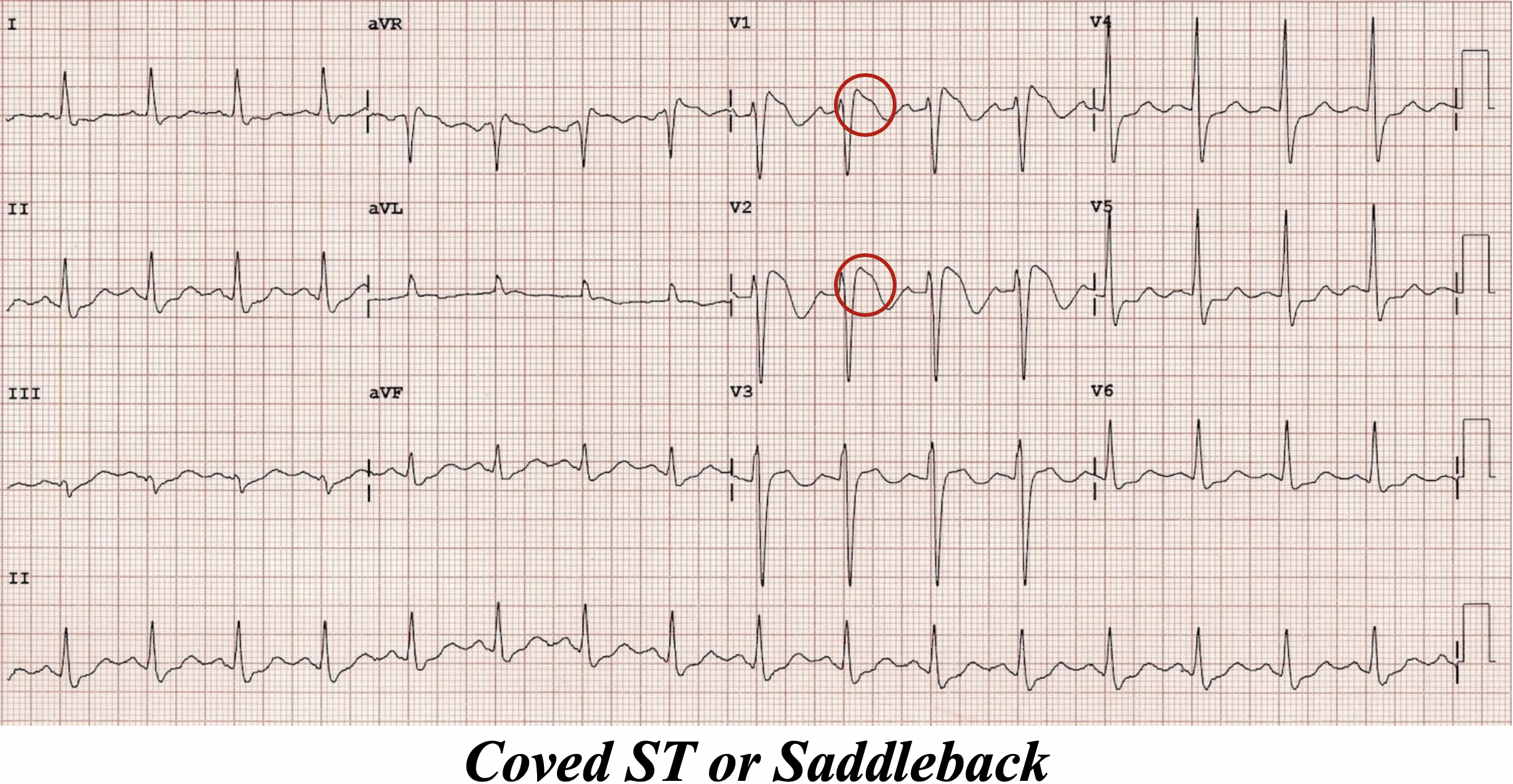
EKG#3
41 year old female, sent from methadone clinic for nausea. Given Zofran at the clinic. Was acting belligerent at triage and required Haldol. Records show she is currently on azithromycin outpt for recent pneumonia.
You get this EKG right before she goes into cardiac arrest.
1. What the hell happened?
2. How you gonna treat?
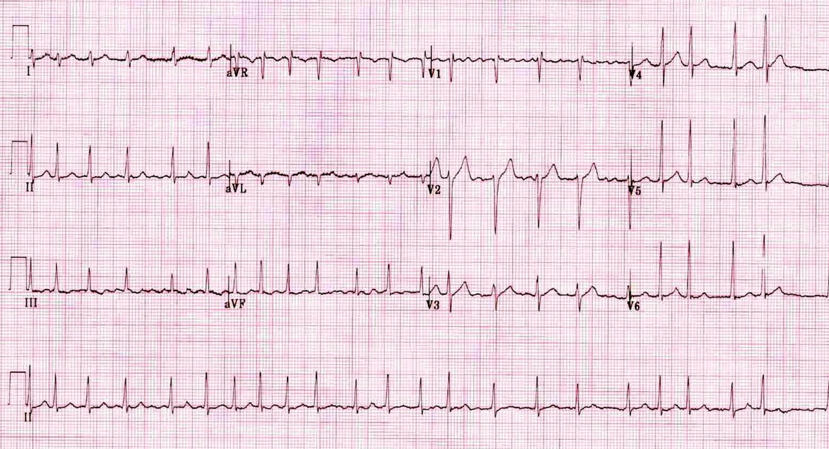
EKG#4
92 year old demented man, wife found him unresponsive near an open medicine cabinet
1. This is a classic dysrhythmia secondary to which toxicity?
2. What is a classic, more subtle finding you can see when the patient in normal sinus rhythm?
ANSWERS
EKGotW #4 – Tox Edition
Brown and University of Cincinnati have amazing reference websites for this topic!
Here are some reference tables from their sites with links that you should totes check out!
http://www.tamingthesru.com/blog/diagnostics/ekg-toxicology, Table by Dr. James Li
EKG#1
Beta Blocker Overdose
1. What’s the rhythm?
a. Junctional bradycardia.
These are QRS complexes without P waves – no P waves means the ventricles are either being triggered from the AV node or more distally (in the actual ventricles).
The complexes are narrow, which means the AV node is likely triggering the impulses, conducting electricity down the bundle of his through the normal conduction pathway.
If the complexes were wide, these might be ventricular escape rhythms – not only do the SA and AV node have their own automaticity, but the actual myocytes themselves may trigger impulses as well.
1. What’s the differential for bradycardia?
a. H.I.D.E.
i. Hypothyroid/Hypothermia
ii. Ischemia/Increased ICP
iii. Drugs
iv. Electrolytes (K, Ca, Mag)
2. Think tox – now narrow your differential. What do the vitals suggest?
a. Several toxidromes may cause severe bradycardia. Commonly we talk about calcium channel blockers and beta blockers. (Don’t forget digoxin from David Elkin’s M&M a few weeks ago!)
Classically, hypoglycemia + bradycardia = beta blocker overdose.
Beware of bronchospasm as a clue as well.
3. How do you want to treat this patient?
a. Glucagon – increases intracellular cAMP and calcium
i. Give with Zofran!
b. Calcium – increase inotropy
c. Epi Drip – for cardiogenic shock
d. High Dose Insulin – 1u/kg/hr, 30-60 min to take effect
e. Lipid Emulsion Therapy – uncertain mechanism
f. Atropine / Pacing can be considered – atropine often ineffective. (Remember, atropine counteracts excessive vagal stimulation, but this is not the etiology of bradycardia in BB OD patients!)
My fave article on this:
https://emcrit.org/pulmcrit/epinephrine-atropine-bradycardia/
EKG#2
TCA Overdose
1. Rate, rhythm, axis, intervals
a. Rate = QRS x 6 = 21 x 6 = 126
b. Rhythm – You can see P waves hiding in I, V5/V6, and maybe small irregularities in the T waves of V3/V4 that hint at presence of P waves. This is sinus.
c. Axis - Downward deflection in I, upward in aVF = RIGHT AXIS
d. Intervals
i. PR < 200msec
ii. QRS > 120msec
iii. QTc = QT/Ö(RàR’) = 0.312 / Ö0.48 = 450msec
^^^(I used V2 for this)
Sinus tachycardia with RIGHT AXIS deviation and WIDE QRS complex
2. What’s the suspected overdose?
a. Hallmarks of TCA Overdose EKG
i. Widened QRS
ii. Big-ass R wave in aVR
iii. New right axis
iv. Deep slurred S waves, I & aVL
3. Treatment?
a. Sodium Bicarb pushes
i. Until the QRS narrows
b. Lidocaine for refractory arrythmia
Read about TCA -- http://www.emdocs.net/ecg-pointers-tca-overdose/
Video about TCA -- https://emin5.com/2015/12/22/tca-toxicity/
EKG#3
Long QT
1. What the hell happened?
a. Haldol, azithromycin, methadone are all QT prolonging agents, which predispose to Torsades de Pointes, or Polymorphic Ventricular Tachycardia
b. Using V5…
QTc = QT / (Square root of R->R’) = 0.74 / (SqRt(1.08) = 711msec
2. How you gonna treat?
a. Defibrillate if in arrest
b. 2g Mag Sulfate slow IV push
c. Isoproterenol +/- pacer if super brady
This case: http://hqmeded-ecg.blogspot.com/2014/06/acquired-long-qt-do-not-trust.html
Torsades overview: https://wikem.org/wiki/Torsades_de_pointes
EKG#4
Digoxin Toxicity
1. Classic Findings
a. This is Bidirectional V-Tach, classic for digoxin toxicity
b. Like David Elkin talked about a few weeks ago in M&M, lots of different arrhythmias possible with digoxin
c. Beware of atrial arrythmias and dangerous bradycardias
d. Classic EKG finding of scooped, down-sloping, Salvador Dali moustache ST segment
Remember the theoretical phenomenon of stone heart – dig tox may give you hyperK. When you treat with calcium, the theory is that it may cause tetany of the myocardium and precipitate cardiac arrest. Digifab (antidote) will treat hyperK, so consider your options.
Dig Toxicity EKG - https://litfl.com/digoxin-toxicity-ecg-library/
Treatment - https://www.wikem.org/wiki/Digoxin_toxicity
References
https://litfl.com/tricyclic-overdose-sodium-channel-blocker-toxicity/
http://brownemblog.com/blog-1/2018/6/20/the-poor-mans-tox-screen
http://www.tamingthesru.com/blog/diagnostics/ekg-toxicology
http://hqmeded-ecg.blogspot.com/2014/06/acquired-long-qt-do-not-trust.html