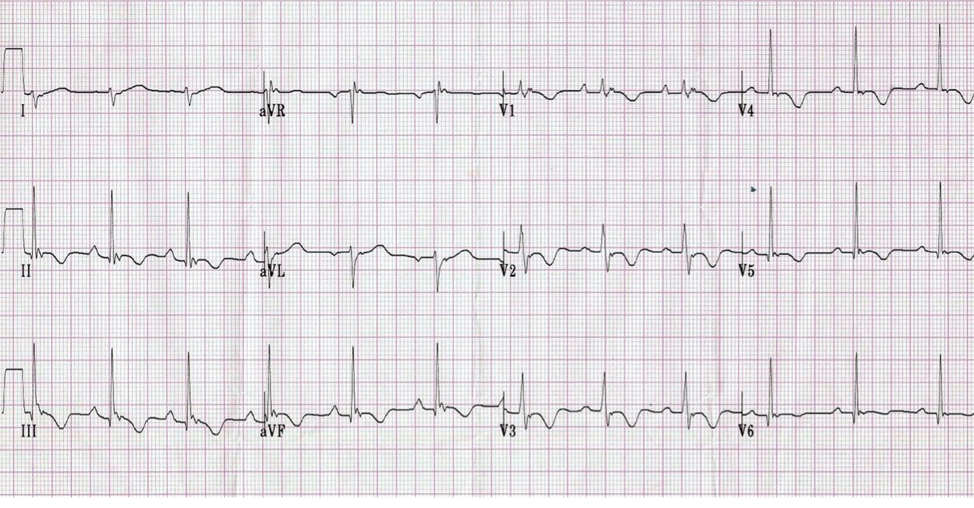
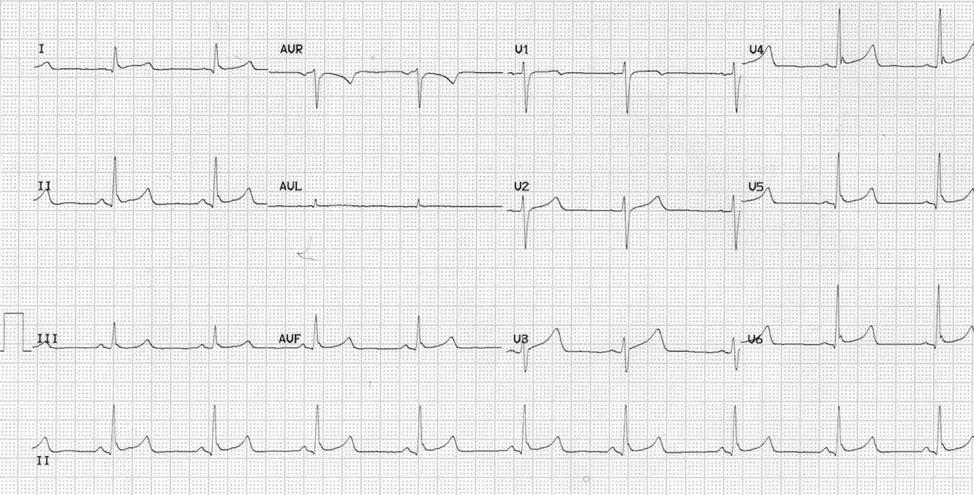
EKG #2 - Multifocal Atrial Tachycardia (MAT)
· Multiple foci in the atria triggering the AV node. Look at all the different P wave shapes!
· Three separate P wave morphologies = diagnostic of MAT
· The slow version of MAT is a wandering pacemaker (MAT without the T)
· Classically presents in a patient with COPD or CHF
· Note that this EKG has R axis deviation, perhaps from cor pulmonale
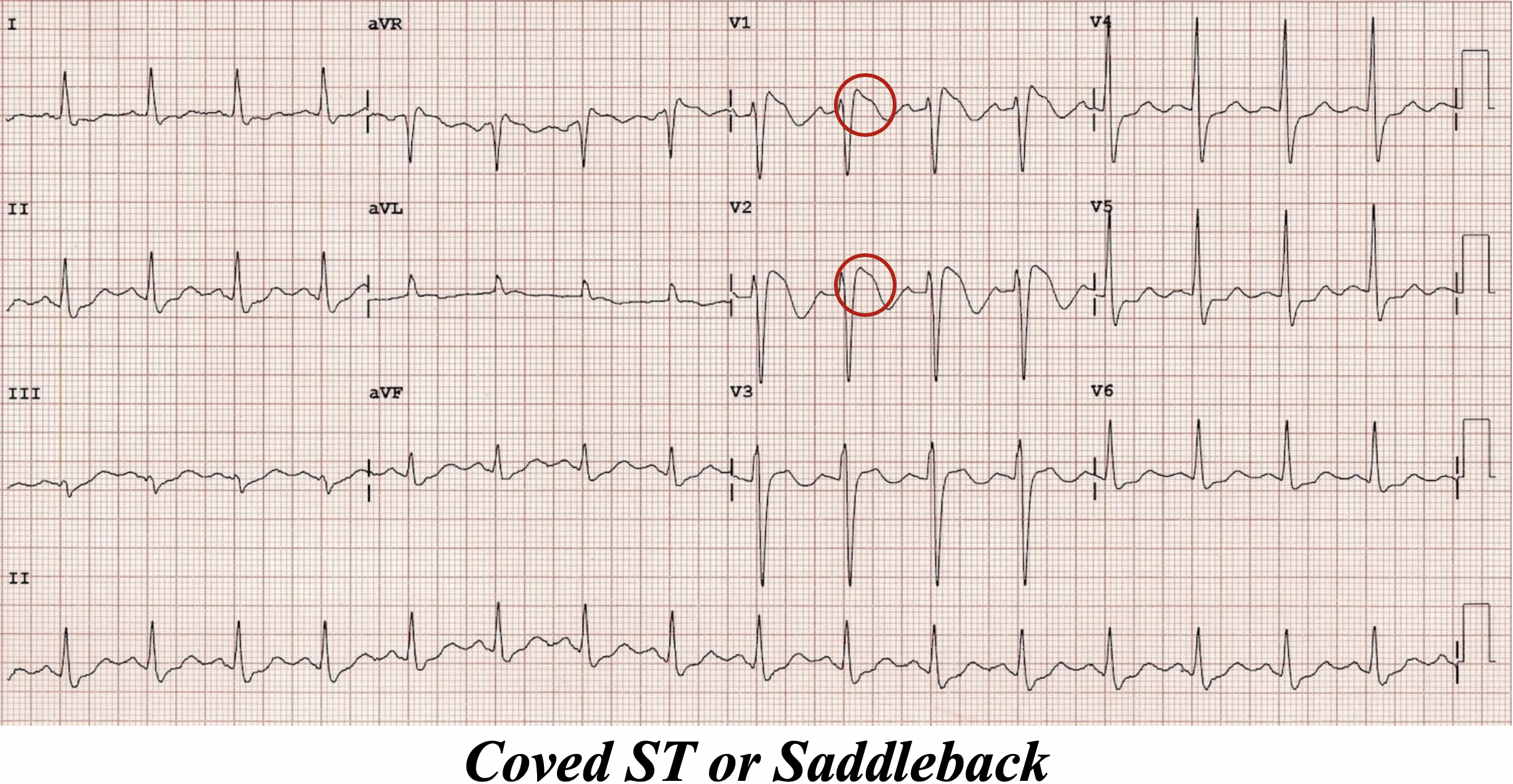
EKG #3 - Premature Atrial Contractions, Normal Sinus Rhythm
· So this is yet another irregularly irregular EKG, and at first glance you may call this atrial fibrillation.
· However, note all the well defined p waves – this is sinus tach
· So why is it irregular?
· Before those irregularly occurring QRS complexes, there is a p wave, and it looks exactly the same as all the other p waves (in height, width, and axis)
· The SA node is firing early, depolarizing the ventricles, and creating an irregular rhythm
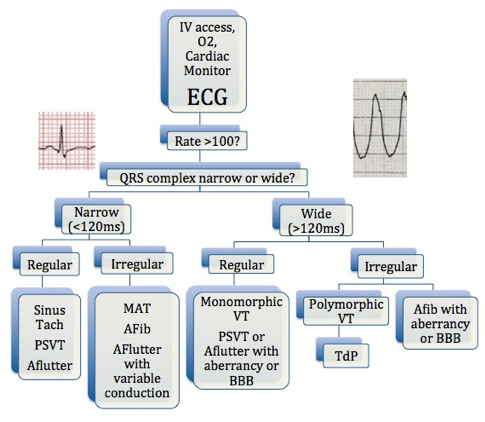
What is a Lewis Lead?
Ohmygod, great question, so glad you asked!
From Wikipedia: “A Lewis Lead is a modified ECG lead used to detect atrial [activity] when [it] is suspected… but is not definitively demonstrated on the standard 12 lead ECG.”
So you think someone has atrial flutter (sustained HR of 145 perhaps?) but you can’t see any p waves or sawtooth activity.
Maybe you’re trying to discern SVT from fast sinus tach?
How can you solve this conundrum?
Lewis Lead!