lets talk about two STEMI equivalents, this post covers De winters, Wellens, hypokalemia, hyperkalemia, to jump to a section look for the BOLDED headers
De Winter T waves
Indicates an acute proximal LAD occlusion
J point depression of 1-3mm
tall wide symmetric T waves
present in precordial leads v2-6
usually 0.5-1mm elevation aVR

Wellens syndrome
indicates acute or chronic proximal LAD stenosis
may present after chest pain
type A symetric isoelectric t waves in V1-2
type B has deep symetric T waves in V1-2
T changes maybe all the way to V6
typically without ST elevation
chest pain is often resolved
Do NOT stress test* patient has no collaterals patient requires catheterization!
type A:
type B:
*there are case reports of large anterior MI's after stress tests
Hypokalemia
Lengthened PR interval
T flattening/inversion
ST depression which can mimic ischemia
U waves after inverted T waves making the appearance of prolonged QT
Ectopic atrial and ventricular beats
Will progress to afib, vtach, vfib, or torsades de pointes


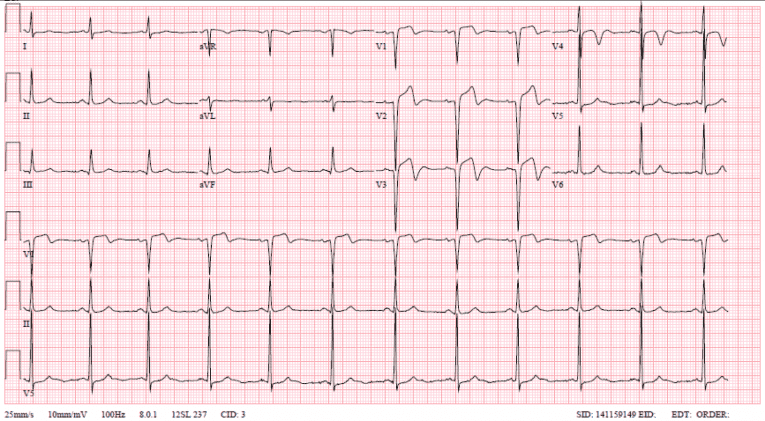
Hyperkalemia
prolonged PR
shortened QT
flattened P waves
Wide QRS
sharp symmetric peaked T waves
can have heart block ventricular arythmias
progresses to sinusoidal wave of WRS and peaked T and cardiac arrest











