First steps (stable pt)
-treat as a trauma pt (ABCDE) and look for traumatic injuries
-place pt on NRB with O2 to 15 L/m
—add nebs 4% lidocaine early to prepare for visualization of cords with videolargynoscope
–4:2:1 rule for burn pt fluid resuscitation
—give fluids even if no external burns visible, as pt will have insensible losses
-treat pain!
-evaluate cords and surrounding laryngeal structures for edema with video laryngoscope or bronch
How to risk-stratify your patient with suspected smoke inhalation injury:
Rule out
–carbon monoxide toxicity: obtain serial blood gases (send co-oximetry) to monitor carboxyHb. Normal levels are 5 – 12%, depending on whether or not the pt is a smoker. Also consider if family presents with similar vague symptoms.
-cyanide toxicity: cyanide levels are not reliable in excluding toxicity, as it is rapidly cleared, and don’t result for days. Use lactate>8 or rising lactate despite fluid resuscitation to raise suspicion for toxicity
—ddx for elevated lactate (=impaired tissue oxygenation) in burn pt: cyanide, metHb, hypoxia, volume depletion
-look for rhabdo and AKI
Warning signs of respiratory failure
–drooling or difficulty swallowing = impending failure
-monitor for stridor, hoarseness, and respiratory distress
-PaO2/FiO2 ratio indicates degree of pulmonary shunting past injured lung. PaO2/FiO2<300 forewarns respiratory failure
Intubation
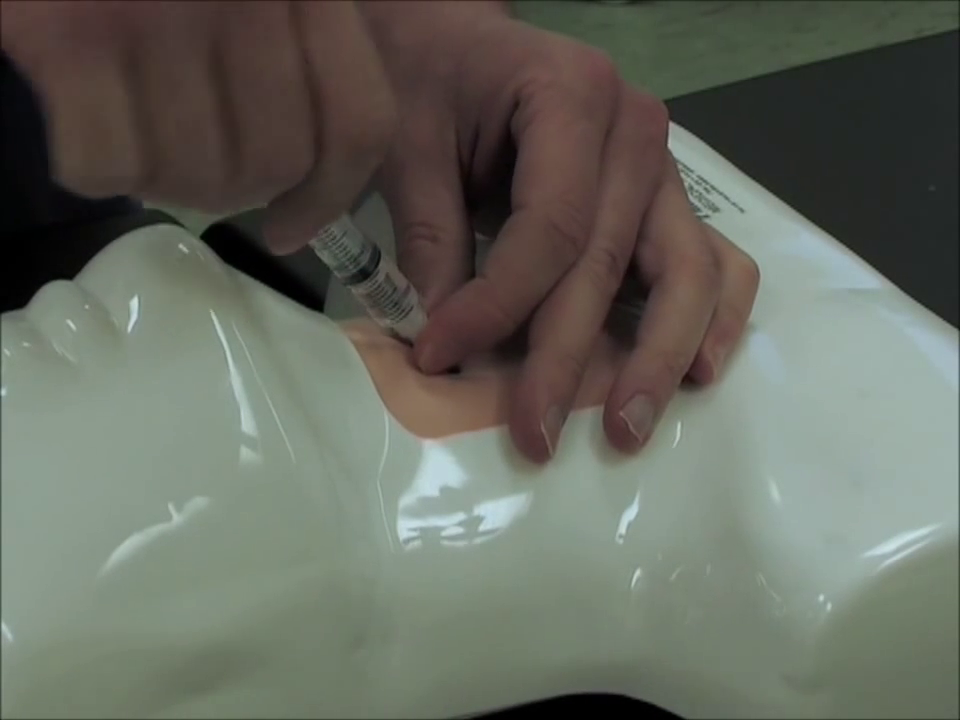
-early elective intubation in a controlled setting is better than crash intubation of a pt with edematous airway structures
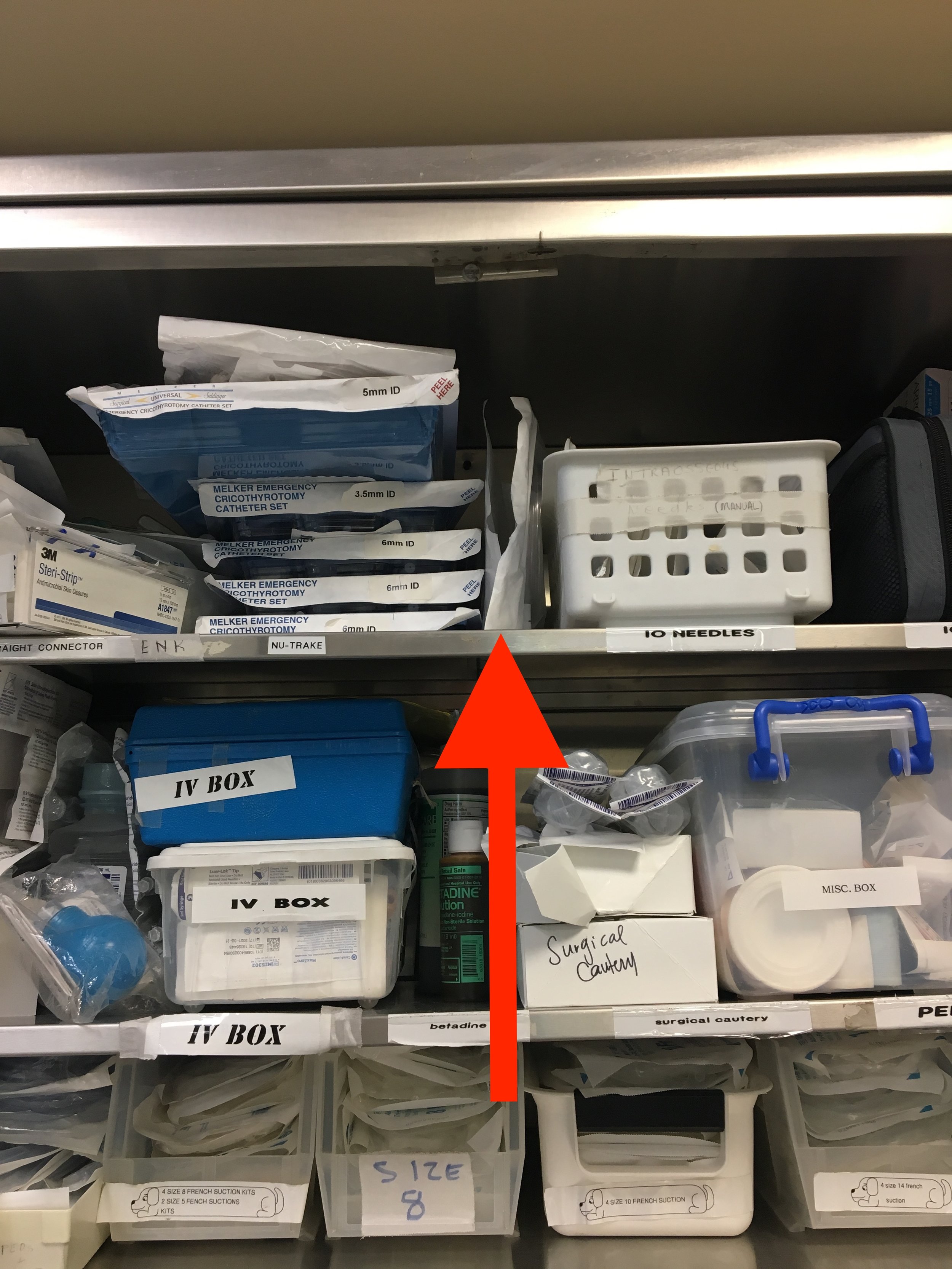
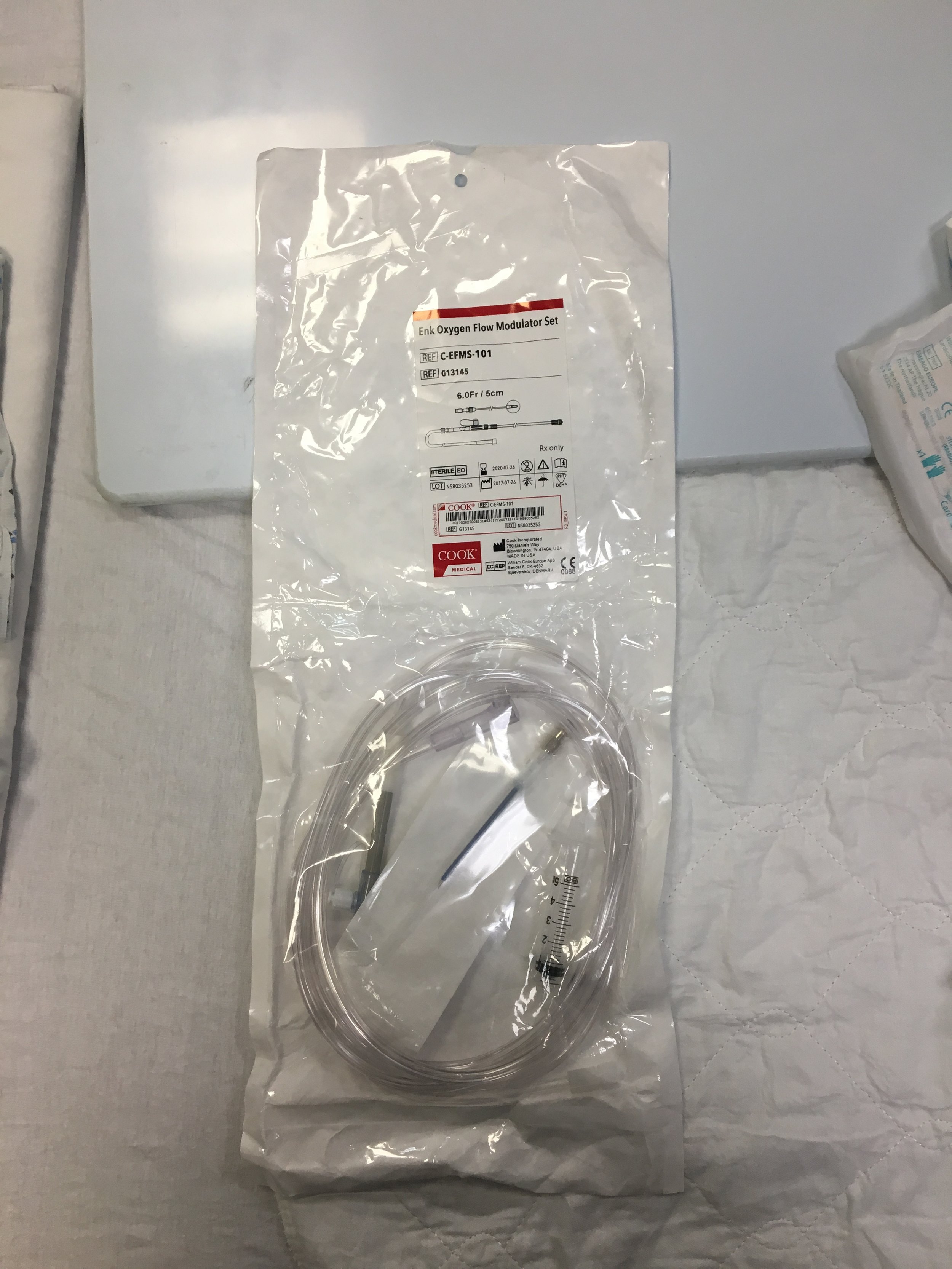
-Prepare multiple sizes ETTs in anticipation of vocal cord edema. Use the largest that will fit so that the pt can get a bronchoscopy upstairs. Prepare suction for soot-filled secretions. Sux is safe to use up to 24h post-burn.
-use volume controlled ARDS settings (6-8 mL/kg TV)
—airways and lung become less compliant in inhalational injury, so must prevent barotrauma and allow for permissive hypercapnea