HPI
A 74-year-old female with a PMH of HTN, scoliosis, and stroke presents to the ED for worsening generalized weakness and poor appetite for 5 days. The patient is tachycardic, tachypneic, and hypoxic to 88%. Her most recent echocardiogram less than a year ago showed a LVEF of 51-55%.
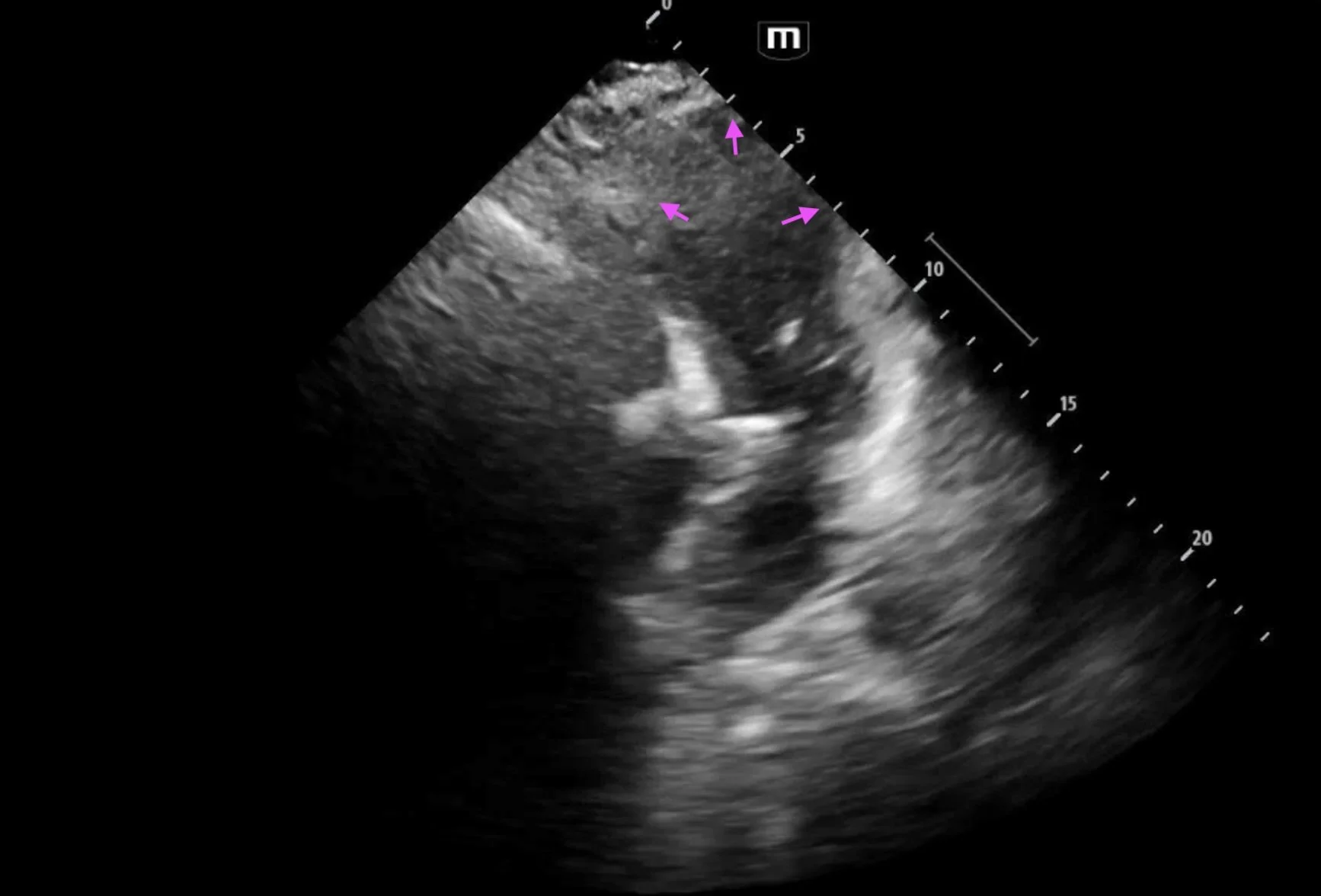
Ultrasound Findings
Bedside echocardiogram showed abnormal wall motion, specifically apical ballooning of the left ventricle
The diagnosis of Takotsubo cardiomyopathy relies on two main criteria:
1) Transient left ventricular wall motion abnormality
2) The absence of a condition obviously explaining this wall motion abnormality
The classic pattern on ultrasound is akinesis of the apex accompanied by hypercontractility of the base, causing an appearance of systolic “ballooning” of the apex. This occurs in 80% of cases; however other variants exist.
Regional wall motion abnormalities extend beyond the distribution of any single coronary artery, sometimes helping differentiate this condition from MI.
Serial echos may show changes in these abnormalities over time.
LV outflow tract obstruction may complicate this condition, causing hemodynamic collapse.
Case Conclusion
ED workup revealed an elevated troponin and BNP, influenza B positive, and the patient was admitted given concern for myocarditis versus ACS.
A comprehensive echo was performed, showing a LVEF of 21-25% and findings consistent with Takotsubo cardiomyopathy. A CTA coronary scan was also performed, showing no evidence of significant CAD. The patient had a complicated hospital course but was medically optimized and ultimately discharged.
References