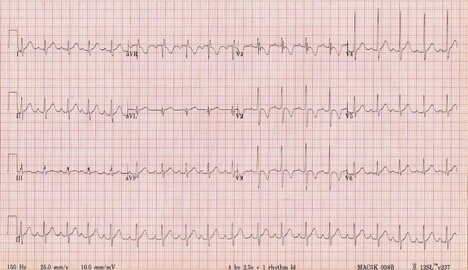
EKG#1
2yoF with fever. There was a miscommunication and someone accidentally got this EKG – even no one asked for it. Many emails have been sent as a result, swaths of staff fired and ridiculed… but even still, you’re stuck with this EKG.
1. Is this 2yo having an MI? Spontaneous coronary artery dissection? Coronary aneurysm from Kawasaki?
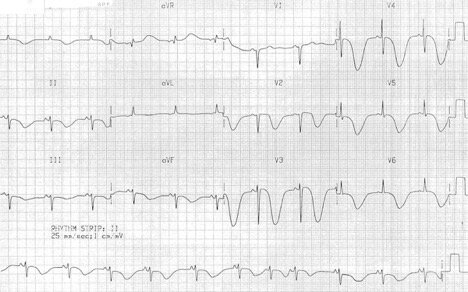
EKG#2
48yoM with exertional chest pain. He’s wearing a fedora and sunglasses indoors. Is this clinically relevant? You decide.
1. Iunno, what do you think? Good? Bad?
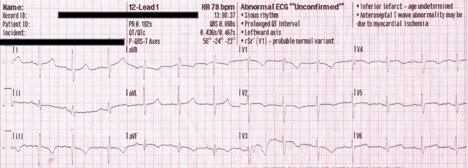
EKG#3
88yoF found unresponsive in the bathroom. No cardiac history.
1. Which came first, the EKG or the fall?
EKG#4
33yoM, exertional SOB
1. Do you agree with the computer interpretation?
2. What test will your order next?
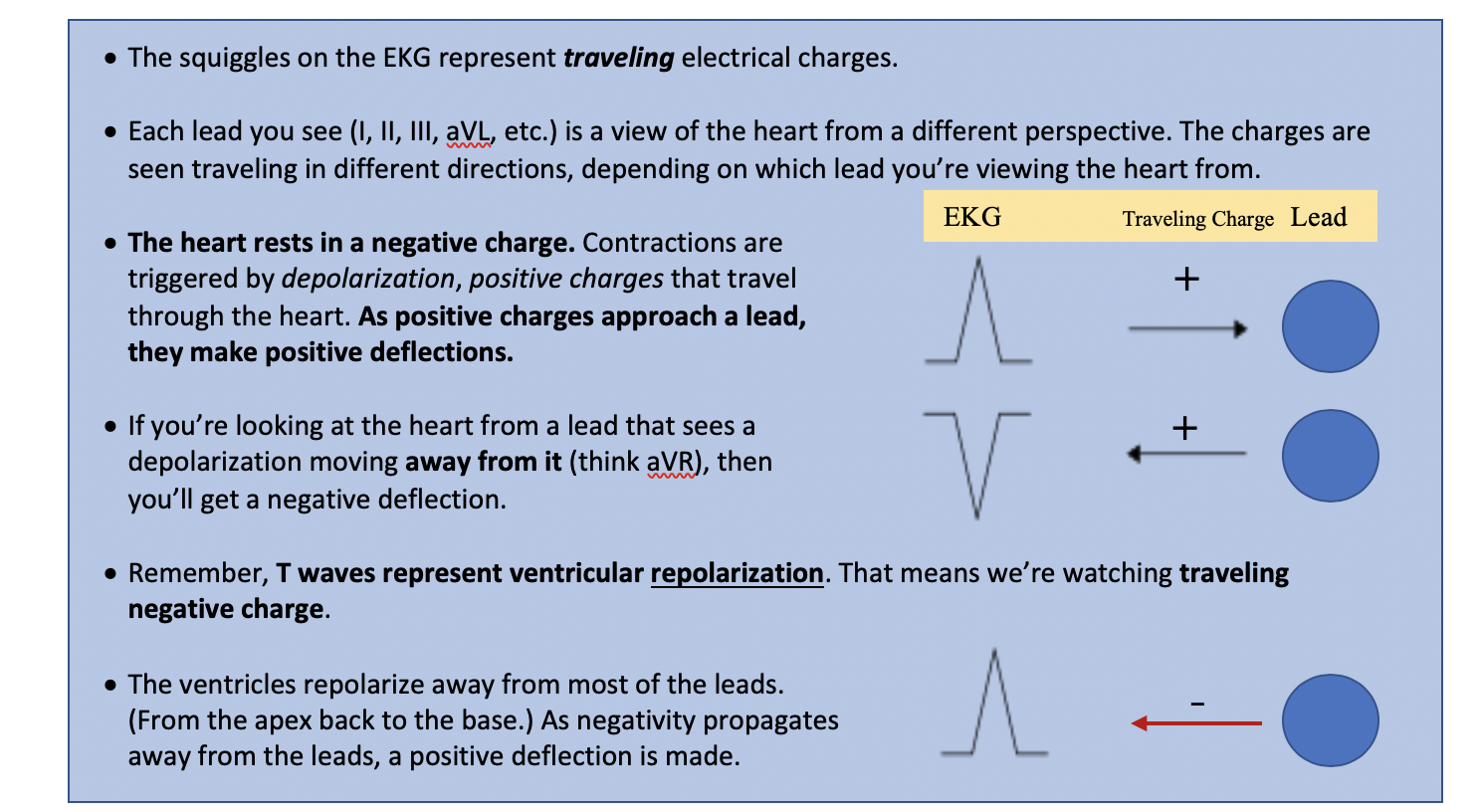
PRECORDIAL T-WAVE INVERSIONS (TWI) EDITION
What’s the differential?
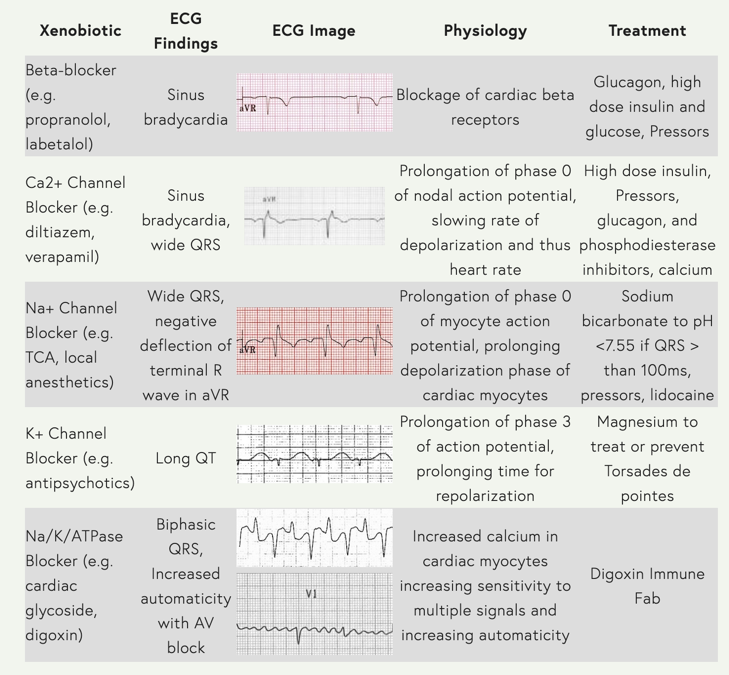
Wow, look at this snazzy graphic you can reference!
Before we start…
…let’s review normal T waves.
T waves should be…
1. Upright in all leads except aVR and V1 (sometimes V2)
2. Asymmetric, with a gradual upslope and a steep return to baseline
3. Smaller than the QRS
Lots of things can invert your T waves
· We will focus today on the differential on the first page
· In addition to these dangerous pathologies, consider…
o Ventricular strain
o HCM
o Lead placement: https://litfl.com/ecg-limb-lead-reversal-ecg-library/
ANSWERS
EKG#1
2yoF with fever – Juvenile T Waves
· Remember, TWI is a normal finding in children.
· Note that these TWI’s are asymmetric, as opposed to the next pathologic example.
o They have a gradual upslope, steep downslope
· They may become upright as early as age 8, or they may “persist” into adulthood.
· Persistent Juvenile T Waves (PJTW) typically present African American women <30yo
but…
· As Dr. Richard Wang said, PJTW is a diagnosis of exclusion. It’s reasonable to interpret this TWI pattern as normal in a child, but consider this pathologic on the adult side until proven otherwise.
From Richard:
· Remember right axis deviation is normal in pediatrics – remember that the R side of the heart does most of the work in-utero, so it’s normal to expect it to be [relatively] bulkier
· This EKG shows “early transition,” meaning R > S in V1/2, suggestive of increased work in the R side of the heart
Additional Reading: https://pedemmorsels.com/pediatric-ecg/
EKG#2
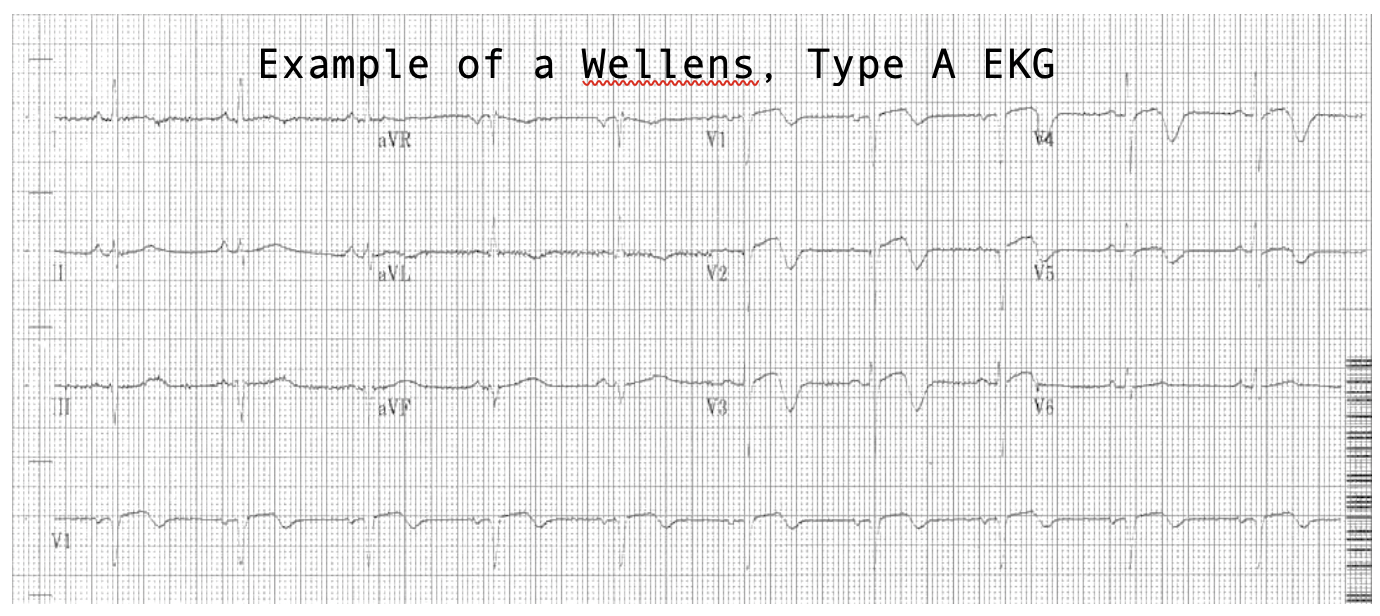
48yoM with exertional chest pain – Wellens, Type B
· Deep, symmetric TWI in the precordial leads = Wellens, Type B
· There are two types of Wellens patterns, A and B.
· Both indicate critical stenosis of the LAD and these patients should be treated as impending STEMI’s, though their ST segments may appear normal.
Here is a fantastic explanation of Wellen’s physiology from Life in the Fast Lane:
· A sudden occlusion of the LAD, causing a transient anterior STEMI. The patient has chest pain & diaphoresis. This stage may not be successfully captured on an ECG recording.
· Re-perfusion of the LAD. The chest pain resolves. ST elevation improves and T waves become biphasic or inverted. The T wave morphology is identical to patients who reperfuse after a successful PCI.
· If the artery remains open, the T waves evolve over time from biphasic to deeply inverted.
· The coronary perfusion is unstable, however, and the LAD can re-occlude at any time. If this happens, the first sign on the ECG is an apparent normalisation of the T waves — so-called “pseudo-normalisation”. The T waves switch from biphasic/inverted to upright and prominent. This is a sign of hyperacute STEMI and is usually accompanied by recurrence of chest pain, although the ECG changes can precede the symptoms.
· If the artery remains occluded, the patient now develops an evolving anterior STEMI.
· Alternatively, a “stuttering” pattern may develop, with intermittent reperfusion and re-occlusion. This would manifest as alternating ECGs demonstrating Wellens and pseudonormalisation/STEMI patterns.
Additional Reading: https://litfl.com/wellens-syndrome-ecg-library/
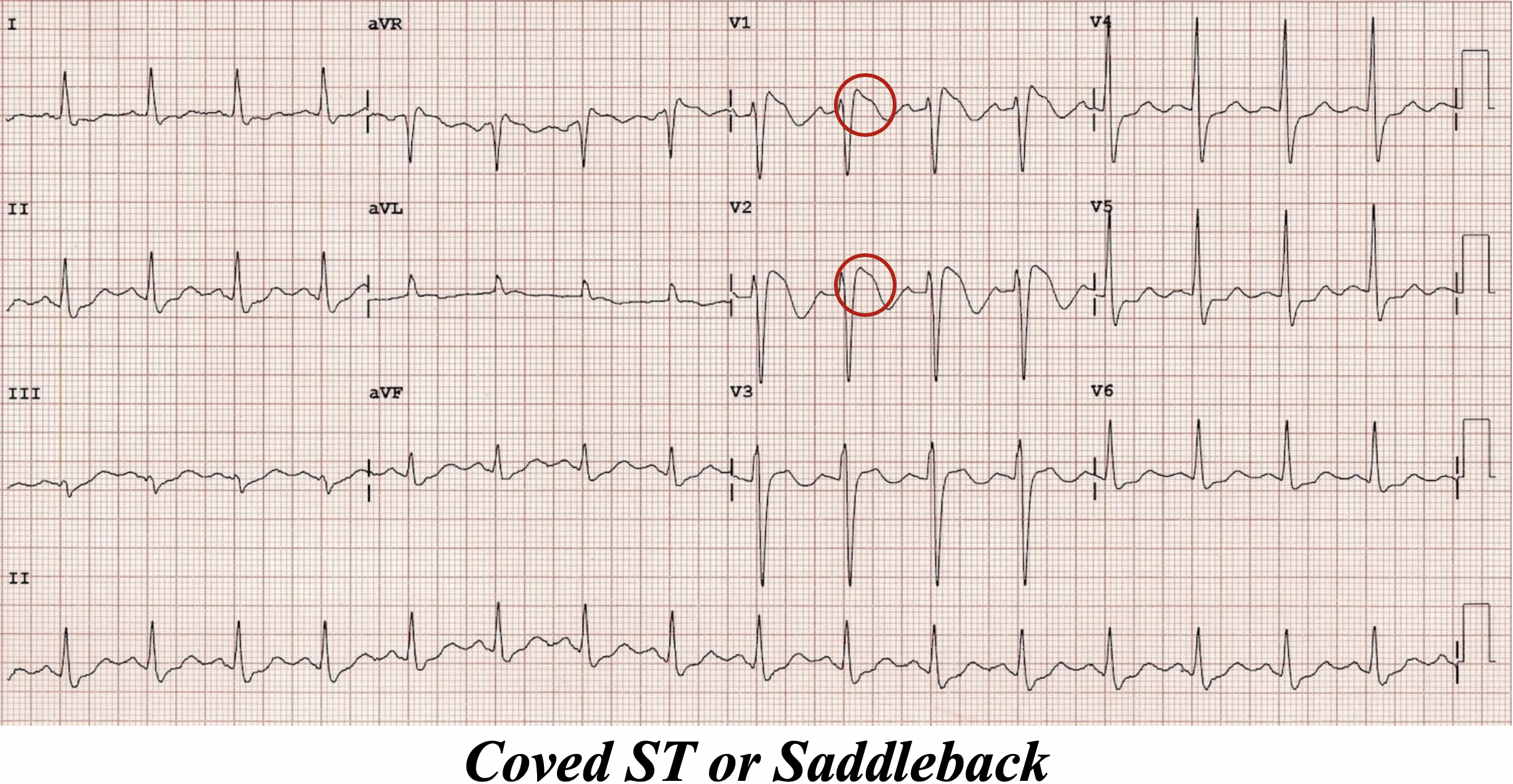
EKG#3
88yoF found unresponsive in the bathroom – Cerebral T Waves
· Deep, SYMMETRIC TWI… are we sensing a pattern here?
· This is a pretty rare phenomenon that occurs with stroke or increased ICP (think bleed).
· This particular EKG is from a patient with a subarachnoid hemorrhage.
· The pathophysiology is currently not known.
· One study (https://www.ajconline.org/article/S0002-9149(17)31597-7/fulltext) found 2% of stroke patients had inverted T waves, and 18% of those had transient wall-motion abnormalities, suggesting that this finding may actually reflect true cardiac dysfunction.
· It is common for stroke patients to spill troponin, so add ‘em on!
Additional Reading: http://www.emdocs.net/ecg-pointers-intracranial-hemorrhage/
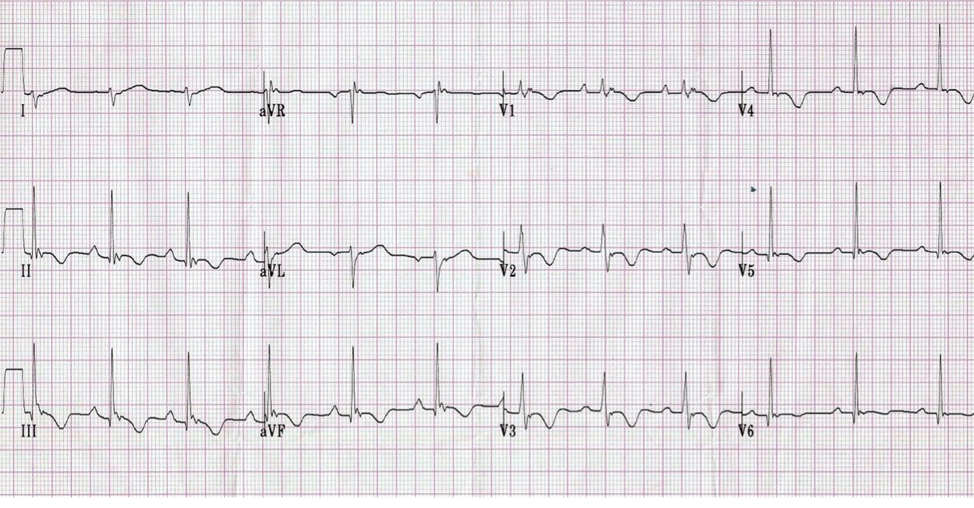
EKG#4
33yoM, exertional SOB – Pulmonary Embolism
· TWI is more prevalent in PE than S1Q3T3, but still not totes specific
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5306533/
· Remember that EKG in PE may be:
o STONE COLD NORMAL
o Sinus Tach
o RBBB
o New Right Axis Deviation
· Great EMCRIT article on how to differentiate AMI from PE:
https://emcrit.org/pulmcrit/two-ekg-patterns-of-pulmonary-embolism-which-mimic-mi/
References
https://litfl.com/ecg-changes-in-pulmonary-embolism/
http://ems12lead.com/2014/11/18/anterior-t-wave-inversions-and-pe/#gref
https://litfl.com/paediatric-ecg-interpretation-ecg-library/