Don’t tell A FIB about SVT. You’ll make my heart FLUTTER.
We're interrupting your weekly emails from EMS extraordinaire Dr. Dave Eng to bring you some guest posts. This week we will be discussing EMS protocols for three tachyarrhythmias: 1) A.fib + A.flutter, and 2) SVT
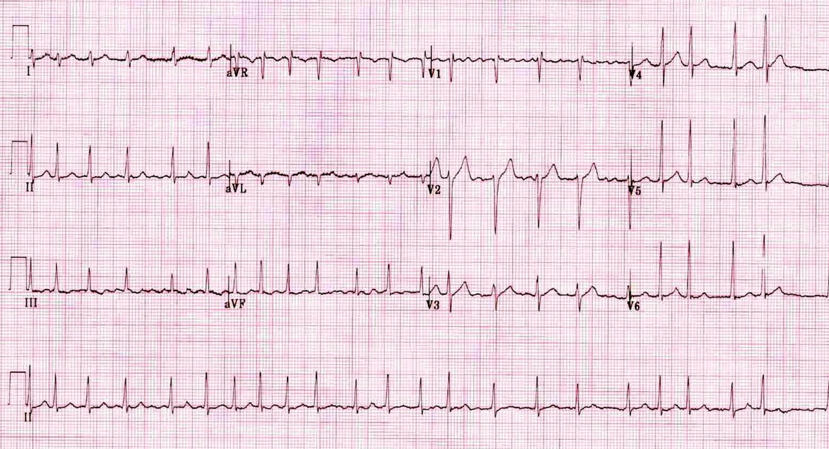
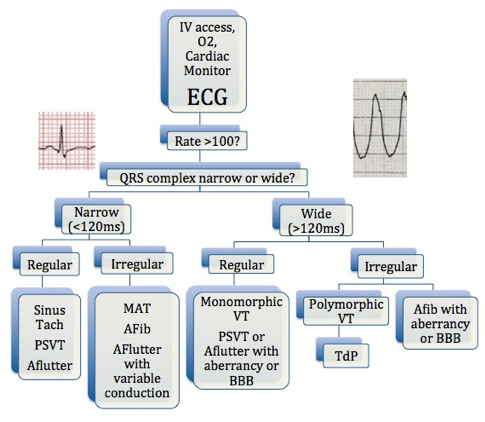
1) Atrial Fibrillation / Atrial Flutter
First question: is this patient stable or unstable? If this patient is hypotensive, altered, or has signs of hypoperfusion, this is an unstable patient. Standing Order will allow paramedics on scene to perform SYNCHRONIZED CARDIOVERSION up to 4 times (first 100J, then 200J, then 300J, then 360J). If that does not work, they will call OLMC for one of two options: administration of Amiodarone 150mg IV or repeating SYNCHRONIZED CARDIOVERSION at max joules setting.
If the patient is stable, there are no Standing Order available so paramedics will call OLMC for one of three options: IVF 10 ml/kg IV, Diltiazem 0.25 mg/kg IV, or Amiodarone 150mg IV. Before authorizing, first assess whether their tachyarrhythmia is compensatory for another cause (i.e. hypovolemia, sepsis, etc.) that may be better addressed first before addressing the rhythm. Choosing what to authorize is dealer’s choice, but typically IVF or Diltiazem is the safest. Diltiazem is great if there is a narrow-complex tachycardia in an otherwise stable patient. I’ve successfully converted a patient with Diltiazem who subsequently arrived at our ED in normal sinus rhythm 15 minutes later. Amiodarone is another option, however has some major side affect profiles as we know. Thoughts are it might help control rhythm while being gentler on the blood pressure in comparison to Diltiazem.
2) SVT
First question again: stable or unstable? If unstable, Standing Order allow paramedics to perform SYNCHRONIZED CARDIOVERSION up to 4 times (first 100J, then 200J, then 300J, then 360J). If the patient is stable, Standing Order allows administration of Adenosine 3 times (first 6mg, then 12mg, then 12mg). If these orders don’t work for both stable or unstable SVT, paramedics will contact OLMC for Diltiazem 0.25mg/kg IV or Amiodarone 150mg IV.
Check out www.nycremsco.org or the protocol binder on North Side for more.
Sincerely,
Joseph Liu, DO
Chief Resident, Emergency Medicine PGY-3
Maimonides Medical Center