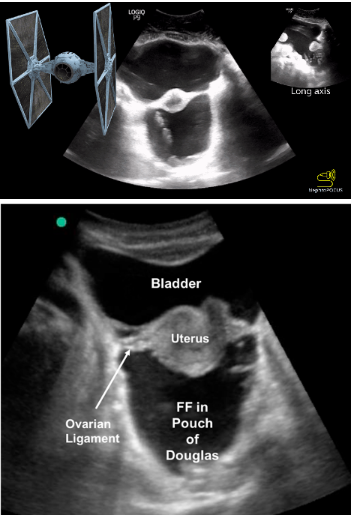
Case: 29 yoF G1P0 presented to the ED with vaginal bleeding and abdominal pain. A transabdominal ultrasound was performed that did not show a definitive IUP. Beta-HCG was elevated at ~30,000. The providers then performed a TVUS that showed a gestational sac without a clear yolk sac and a concerning second structure (video 1). OBGYN was consulted to rule out ectopic pregnancy and their repeat US showed an IUP. However, they also identified 2 uteruses and a vaginal septum, leading them to believe that the patient had uterus didelphys.
Video 1: Superficially you see a collapsed bladder. On the right side of the video, you see 1 uterine horn with a thickened endometrium and no gestational sac. On the left side of the video, towards the end of the clip, you can see an endometrium with a gestational sac.
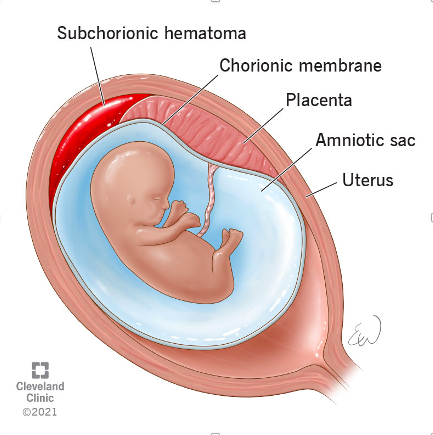
Uterus didelphys is a rare condition where a person develops 2 uteruses. It occurs when the Mullerian ducts do not fuse during embryologic development, resulting in 2 separate uteruses, each with its own fallopian tube and ovary (image 1). Some people also have 2 cervixes and 2 vaginal canals. This condition occurs in 0.3% of the population. Pregnancies in women who have uterus didelphys are considered high risk as there is less room for fetus to develop.
Case conclusion: the patient was counseled about risks and the need for close follow-up. She has a repeat ultrasound and appointment in the outpatient clinic this week.
Happy Scanning!
- Ariella Cohen, MD
References: https://my.clevelandclinic.org/health/diseases/23301-uterus-didelphys